- Visibility 67 Views
- Downloads 2 Downloads
- DOI 10.18231/j.ijpo.2024.030
-
CrossMark
- Citation
Oral squamous cell carcinoma: Histological grading and co relationship with cervical metastasis, depth of invasion and perineural invasion
- Author Details:
-
Sheeba Parvez
-
Bazila Mansoor *
-
Rimsha Ahmed
-
Arvind Khajuria
Introduction
Around, 95% of the cancers of the head and neck are known to be squamous cell carcinomas.[1]
A WHO report in 1983 stated that, oral cancer is the most common cancer in southeast asia. Most common traditional risk factors of oral cancers are tobacco and alcohol abuse.[2] It commonly affects men in the 6th to 8th decades of life and comparatively lesser cases occur in patients younger than 40 years.[3] It has a higher incidence in males than females (M: F=1.5:1) mainly because more men as compared to women indulge in habits like tobacco and alchohol abuse.[4] This carcinoma affects all areas of the oral cavity, but tongue, floor of the mouth, and lower lip are the most common reported sites.[3]
The established pre requirements for management are staging and grading of oral squamous cell carcinoma, because they influence risk stratification and personalised treatment.
Broder’s first introduced histological grading for squamous cell carcinomas of lip;it was based on differences in degree of differentiation between tumors.[5] Broder’s suggested a system in which a grade I lesion was highly differentiated (its cells were producing much keratin) while grade IV was poorly differentiated (the cells were highly anaplastic and showed almost no keratin formation). Broder’s initiated quantitative grading in cancer. His classification is based on proportion of the neoplasm resembling normal squamous epithelium and has been used for squamous cell carcinoma for many years altogether.[6]
The metastasis of this carcinoma in cervical lymph nodes has shown to be a major influence on survival in oral cancer in many studies.[7] It is an ominous prognostic factor in head and neck squamous cell carcinoma (HNSCC). Even if there is only one metastatic lymph node, it takes the patients to an advanced stage disease category and also changes the rate of survival of the patient.[8]
The American Joint Committee on Cancer (AJCC) staging system has taken into account numerous factors for nodal metastasis, including size, laterality, and number of malignant nodes. Recently another important factor has been added i.e the extranodal extension (ENE), also called extracapsular spread.[9]
Next parameter is the Depth of invasion(DOI) which is also called reconstructed tumor thickness and differs from clinical tumor thickness, specifically in exophytic and ulcerated lesions. DOI was originaly called as distance from a theoretical reconstructed normal mucosal surface line to the deepest extent of growth of tumor.[10]
Many studies have included investigation on tumor thickness and depth of invasion as prognosis predictors.[11] However, in the literature, the depth of invasion and tumor thickness are often not very clear. According to the American Joint Committee on Cancer Classification (AJCC) 8th edition, DOI is measured from the level of the basement membrane of the closest adjacent normal mucosa. A vertical line is drawn from this plane to the deepest point of tumor invasion.[12] Therefore, depth of invasion is not the same as tumor thickness and neither of the two are interchangeable.[13] Tumor thickness could be larger than DOI in exophytic tumors, and lower than DOI in an endophytic/ulcerated growth pattern. Also, tumor thickness is not shown to be a very good predictive factor.[14]
For a tumor entity explicitily characterised as neurotrophic, it is not surprising that perineural invasion is commonly observed in oral squamous cell carcinoma. If perineural invasion (PNI) is present, it is now widely accepted as an unfavourable prognostic factor.[15], [16]
Perineural invasion is a tropism of tumor cells for nerve bundles in the surrounding tissues. PNI is a type of metastatic tumor spread which is similar to but at the same time distinct from vascular or lymphatic invasion as it hinders the ability to establish local control of a malignancy because neoplastic cells can travel along nerve tracts far from the primary lesion and are often missed during surgery[17] because of this these tumors have the ability to exhibit pain and persistent growth with a long clinical course and late onset of metastases, such a pattern other has been observed in neurotropic tumor such as prostate cancer, pancreatic cancer, melanoma and salivary gland malignancies such as adenoid cystic carcinoma and polymorphous low grade adenocarcinoma. Among all the other parameters used, peri neural invasion is widely known as an indicator of aggressive behaviour.[18] PNI is a well-known independent predictor of poor prognosis in carcinoma colon and rectum and salivary gland.[19]
Materials and Methods
The records of department of Pathology of Acharya Shree Chandra college of medical sciences and hospital were studied retrospectively from November 2020 to February 2023.
A total of 53 cases were found during the time period with age ranging from 27 to 83 years.
All the general information about the case including name, age, date of surgery, surgeon name were registered.
Record of histopathological report of all the 53 cases were studied.
Grading system
Broders system (descriptive system)
Tumors were graded as:
Well- differentiated (Grade 1) = <25% undifferentiated cells
Moderately- differentiated (Grade 2) = <50% undifferentiated cells
Poorly- differentiated (Grade 3) = <75% undifferentiated cells
Anaplastic or pleomorphic (Grade 4) = >75% undifferentiated cells
Results
A total of 53 cases were reviewed during the time period between April 2021 to Jan 2023.
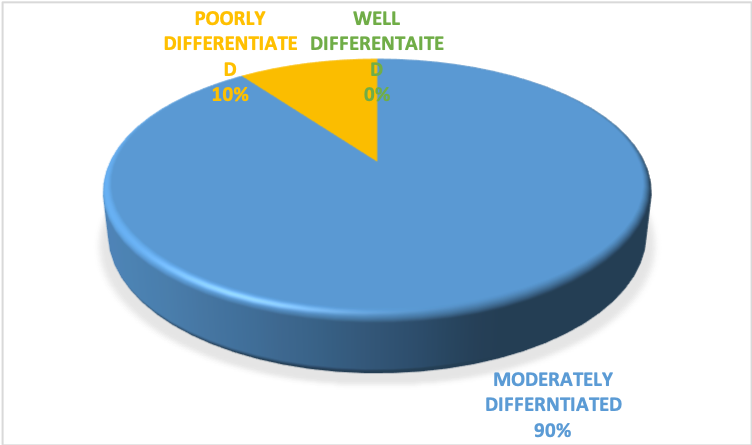
All these cases were diagnosed according to the Broders classification.
Out of 53, there were 23 cases of well differentiated squamous cell carcinoma, 26 cases of moderately differentiated squamous cell carcinoma and 4 case of poorly differentiated squamous cell carcinoma.
First, we assessed the relationship between the histological grading and lymph node metastasis.
We found that, out of 23 cases of well differentiated squamous cell carcinoma, 9 had cervical lymph node metastasis; out of 26 moderately differentiated cancers,14 were found positive for nodal metastasis and out of 4 poorly differentiated cancers 3 had cervical metastasis.
The tabular form of the above data is present below.
|
Grading |
Lymph node metastasis |
|
|
Positive |
Negative |
|
|
Well Differentiated (23) |
9(11.28)[0.46] |
14(11.72)[0.44] |
|
Moderately Differentiated (26) |
14(12.75) [0.12] |
12 (13.25) [0.12] |
|
Poorly Differentiated (04) |
3 (1.96) [0.55] |
1 (2.04) [0.53] |
|
Column total |
26 |
27 |
The chi square stastistic is 2.2227. The p-value is 0.32911. [ The result is not significant at p <.05]
Secondly, we assessed the relation between histological grading and depth of invasion.
We classified the depth of invasion into 3 categories:
Less than or equal to 5mm
Equal to 10mm or less than 10mm and more than 5mm
More than 10mm(6)
We found that out of that out of the 23 cases of well differentiated cancers, 6(26.1%) had a DOI of less than or equal to 5mm, 10(43.5%) had a DOI of equal to or less than 10mm and 7(30.4%) had a DOI of more than 10mm.
Out of the 26 cases of moderately differentiated oral cancers, 1(3.8%) had a DOI of less than or equal to 5mm, 9(34.6%) had a DOI of equal to or less than 10mm, and 16 (61.6%)had a DOI of more than 10mm.
Out of the 4 poorly differentiated cancers, 1 had a DOI of less than or = 5mm; 1 had DOI of more than 5mm and less than or = 10mm, and 2 had a DOI of more than 10mm.
The tabular form of the above given data is present below:
|
Histological Grading |
Less than 5mm OR =5mm |
Equal to 10mm or less than 10mm and more than 5mm |
More than 10mm |
|
Well differentiated(23) |
6(3.47) [1.84] |
10 (8.68)[0.20] |
7 (10.85)[1.37] |
|
Moderately differentiated(26) |
1(3.92) [2.18] |
(9.81) [0.07] |
16 (12.26)[1.14] |
|
Poorly differentiated(01) |
1(0.60) [0.26] |
1(1.51) [0.17] |
2(1.89) [0.01] |
The chi square statistic is 7.231. The p value is .124173. [The result is not significant at p <.05].
Lastly, we assessed the relationship between histological grading and perineural invasion.
We found that out of the 53 cases, 10(18.9%) had been diagnosed with perineural invasion. Moreover, we found that 9 cases were moderately diiferentiated squamous cell carcinomas and 1 case was of poorly differentiated carcinomas.



Discussion
Oral cancer is a serious health problem which has caused a great number of mortality and morbidity through the years. In regions of the world where tobacco habits are practiced in the form of chewing or smoking, OSCC is a major oncological problem.[20]
In the current times, the diagnosis and even the treatment are based on clinical and histo-pathological characteristics of OSCCC. Since many decades, histologic grading is being used in an attempt to predict the clinical behaviour of OSCC.[21]
In clinical practice, the treatment plan and prognosis of OSCC are mainly based on the tumor node metastasis (TNM) (primary tumor, regional lymph node metastasis, and distant metastasis) staging system. But this TNM system does not provide any information on the clinical behavior of the tumor and its biological characterstics.[16]
From the above results, we draw the inference that lymph node metastasis is more prevelant in a higher grade of oral squamous cell carcinomas.
Also, we get to know that higher grades of carcinomas invade more deeply as 16 moderately differentiated cancers invaded deeper than 1cm and only 9 out of 23 well differentiated cancers invaded more than 1cm.
Moreover, we see that perineural invasion is not at all present in well differentiated cancers in our study.
Conclusion
We conclude that breslow grading does relate to regional metastasis, DOI and PNI.
There should be more studies at a larger level to ascertain the potential of Breslow grading.
Source of Funding
None.
Conflict of Interest
None.
References
- V Kumar, AK Abbas, JC Aster. . Robbins & Cotran Pathologic Basis of Disease 2020. [Google Scholar]
- M Akhter, S Hossain, QB Rahman, MR Molla. A study on histological grading of oral squamous cell carcinoma and its co-relationship with regional metastasis. J Oral Maxillofac Pathol 2011. [Google Scholar]
- HC Rai, J Ahmed. Clinicopathological Correlation Study of Oral Squamous Cell Carcinoma in a Local Indian Population. Asian Pac J Cancer Prev 2016. [Google Scholar]
- L Feller, J Lemmer. Oral squamous cell carcinoma: Epidemiology, clinical presentation and treatment. J Cancer Ther 2012. [Google Scholar]
- A Almangush, AA Mäkitie, A Triantafyllou, RD Bree, P Strojan, A Rinaldo. Staging and grading of oral squamous cell carcinoma: An update. Oral Oncol 2020. [Google Scholar]
- G Anneroth, J Batsakis, M Luna. Review of the literature and a recommended system of malignancy grading in oral squamous cell carcinomas. Scand J Dent Res 1984. [Google Scholar]
- JA Woolgar, J Scott. Prediction of cervical lymph node metastasis in squamous cell carcinoma of the tongue/floor of mouth. Head Neck 1995. [Google Scholar]
- L Cerezo, I Millán, A Torre, G Aragón, J Otero. Prognostic factors for survival and tumor control in cervical lymph node metastases from head and neck cancer. A multivariate study of 492 cases. Cancer 1992. [Google Scholar]
- MB Amin, S Edge, F Greene. . AJCC Cancer Staging Manual 2017. [Google Scholar]
- M Pentenero, S Gandolfo, M Carrozzo. Importance of tumor thickness and depth of invasion in nodal involvement and prognosis of oral squamous cell carcinoma: a review of the literature. Head Neck 2005. [Google Scholar]
- MB Amin, FL Greene, SB Edge, CC Compton, JE Gershenwald, RK Brookland. The Eighth Edition AJCC Cancer Staging Manual: Continuing to build a bridge from a population-based to a more "personalized" approach to cancer staging. CA Cancer J Clin 2017. [Google Scholar]
- C Moore, JG Kuhns, RA Greenberg. Thickness as prognostic aid in upper aerodigestive tract cancer. Arch Surg 1986. [Google Scholar]
- SJ Shim, J Cha, WS Koom, GE Kim, CG Lee, EC Choi. Clinical outcomes for T1-2N0-1 oral tongue cancer patients underwent surgery with and without postoperative radiotherapy. Radiat Oncol 2010. [Google Scholar]
- S Spoeri, S Spoerl, S Reil, M Gerken, N Ludwig, J Taxis. Prognostic Value of Perineural Invasion on Survival and Recurrence in Oral Squamous Cell Carcinoma. Diagnostics (Basel) 2022. [Google Scholar]
- AD Rapidis, N Givalos, H Gakiopoulou, G Faratzis, SD Stavrianos, GA Vilos. Adenoid cystic carcinoma of the head and neck. Clinicopathological analysis of 23 patients and review of the literature. Oral Oncol 2005. [Google Scholar]
- VP Wagner, LP Webber, M Curra, IP Klein, L Meurer, VC Carrad. Bryne's grading system predicts poor disease-specific survival of oral squamous cell carcinoma: a comparative study among different histologic grading systems. Oral Surg Oral Med Oral Pathol Oral Radiol 2017. [Google Scholar]
- PM Speight, AW Barrett. Prognostic factors in malignant tumours of the salivary glands. Br J Oral Maxillofac Surg 2009. [Google Scholar]
- RI Haddad, DM Shin. Recent advances in head and neck cancer. N Engl J Med 2008. [Google Scholar]
- . Protocol for the Examination of Specimens from Patients with Cancers of the Oral Cavity . 2017. [Google Scholar]
- BSMS Siriwardena, A Tilakaratne, EAPD Amaratunga, WM Tilakaratne. Demographic, aetiological and survival differences of oral squamous cell carcinoma in the young and the old in Sri Lanka. Oral Oncol 2006. [Google Scholar]
- A Bhargava, S Saigal, M Chalishazar. Histopathological Grading Systems In Oral Squamous Cell Carcinoma: A Review. J Int Oral Health 2010. [Google Scholar]
