- Visibility 23 Views
- Downloads 8 Downloads
- DOI 10.18231/j.ijpo.2022.054
-
CrossMark
- Citation
Changing faces and habitat of mucormycosis epidemic in sequential COVID waves
Introduction
As India continues to battle the COVID 19 pandemic, many new serious complications of the infection have surfaced. The Corona virus poses a greater challenge in the form of the deadly fungal infection mucormycosis. Mucormycosis is a fungus belonging to Phylum Zygomycota, class Zygomycetes, Order Mucorales, family mucoraceae and mucor species.
In early December 2019, the first case of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection were identified in Wuhan and subsequently causing a worldwide pandemic. It is associated with a wide range of disease patterns, ranging from mild to life-threatening pneumonia. A wide range of co-infections exists and may be associated with preexisting morbidities or may develop as a hospital-acquired infection such as ventilator-associated pneumonia.[1]
In the absence of any proven antiviral therapies or vaccines, the glucocorticoids have been shown to reduce mortality in hypoxemic patients with COVID-19.[2] However, glucocorticoids can increase the risk of secondary infections. Moreover, the immune dysregulation caused by the virus and the use of concurrent immunomodulatory drugs such as tocilizumab, an anti-IL-6 therapy, further increases the risk of secondary infections in COVID-19 patients.[3], [4] Few studies described that a significant decrease in lymphocyte count and an increase of neutrophil count along with an inflammatory storm, are related to the severity of the COVID-19 and the associated co-infections.[5]
The combination of COVID-19, corticosteroid therapy and diabetes creates the perfect soil in which mucormycosis takes roots and thrives. It has emerged as a major threat in India as the country carries the high prevalence rate of type 2 diabetes mellitus (8.9% of adults, 77 million patients).[6] Hyperglycemia in patients with diabetes creates an even more favorable environment for the infective organisms. And is now emerging as a well-known risk factor.
Mucormycosis is an infection caused by fungi belonging to the order Mucorales. Rhizopus oryzae is the most common organism isolated from patients with mucormycosis and is responsible for ∼70% of all cases of mucormycosis.[7] The major risk factors for mucormycosis include uncontrolled diabetes mellitus in ketoacidosis, other forms of metabolic acidosis, treatment with corticosteroids, organ or bone marrow transplantation, neutropenia, trauma and burns, malignant hematologic disorders, and deferoxamine therapy in patients receiving hemodialysis.[7]
In addition to host factors that predispose patients to mucormycosis, Mucorales possess virulence factors that enable the organism to cause disease. One such trait is the ability to acquire iron from the host. Iron is an essential element for cell growth and development, contributing to many vital processes of the cell.[8]
The authors discuss the cases of invasive fungal rhinosinusitis, a life-threatening infection, in the patients with COVID-19, encountered in immunocompromised individuals, including those with diabetes mellitus and the varying presentations encountered with each covid wave.
Materials and Methods
A prospective study of 31 patients with history of COVID, sinonasal fungal infection, treated at Tertiary care Medical College was done. The patients were treated according to COVID treatment protocols. Following recovery, these patients presented with sinonasal discharge and infection in ENT and Oral surgery OPD. Diagnosis of Mucormycosis was established after clinical assessment and Magnetic Resonance Imaging. Two patients were treated outside and got admitted in our hospital with complaints of Sino nasal discharge.
Surgical treatment included debridement of the Sinonasal tissue and maxillectomy in three cases. Biopsy specimen was undertaken either by endoscopic or open technique. Patient details were analyzed for clinical presentation, imaging features and histopathological details. Routine hematological investigations, liver and renal function tests, radiological imaging, blood glucose levels were done for all patients. Surgically excised sino nasal biopsy specimen was subjected to a standard fixation protocol and the sections were stained with hematoxylin and eosin (H and E), PAS, and Gomori’s methenamine silver (GMS) stains. Specimens collected in a sterile container without formalin were subsequently sent to the department of microbiology for potassium hydroxide (KOH) examination and fungal culture.
Institutional ethics committee approval was obtained prior to commencing the study.
Results
Demographics
There were 21 males and 10 females, mean age in the study group was 56 years (range 35-75 years). Patients had history of COVID and had presented with Sino nasal discharge in post recovery period. Bilateral nasal cavity involvement was seen in eight cases, while other cases had involvement unilateral side. Interstingly one of the cases presented as acute abdomen diagnosed as intestinal mucormycosis.
Clinical presentations
Nasal discharge, diminution of vision, restricted eye movements, facial pain and swelling were the most common presenting complaints. One patient with Post covid pneumonia and osteomyelitis and left sided nasal discharge was treated but presented with similar complaints of nasal discharge within a span of 10 days. 28 out of 31 patients had history of Diabetes mellitus. Uncontrolled diabetes in these cases may be attributed to ongoing steroid therapy and their long duration of hospital stay. In six patients who underwent maxillectomy for the complaint of diffuse facial swelling, restricted eye movement, clinical diagnosis of Mucormycosis associated osteomyelitis was confirmed histopathologically.
One of the patients post covid recovery was readmitted for acute abdomen. An initial possible diagnosis of enterocutaneous fecal fistula, ischemic colitis was considered clinically. On exploratory laparotomy it was found to have a gangrenous ascending colon and caecum. Excised tissue from inflamed margin of caecum showed numerous fungal hyphae which were histopathologically confirmed to be mucormycosis.
Histopathology
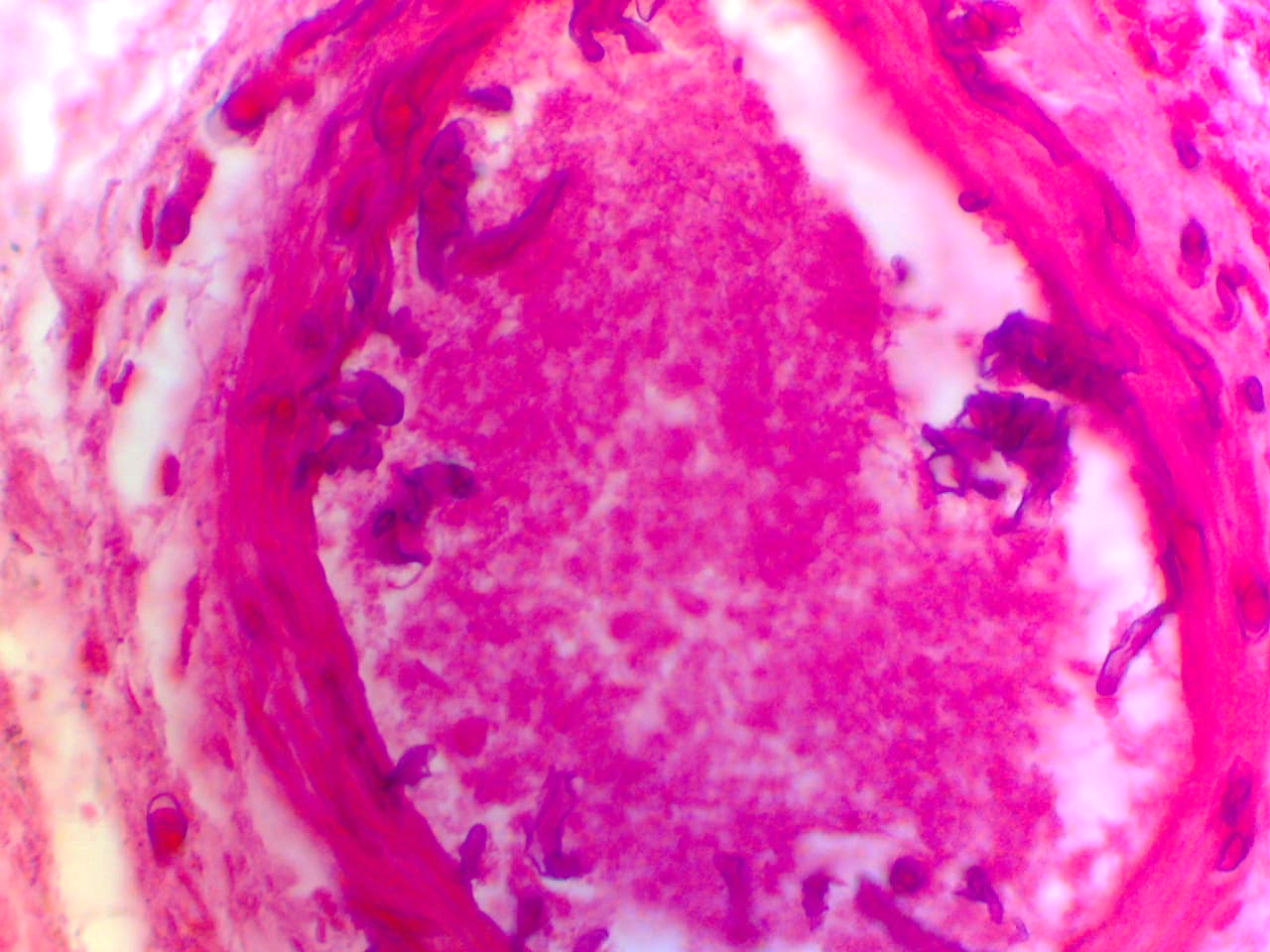
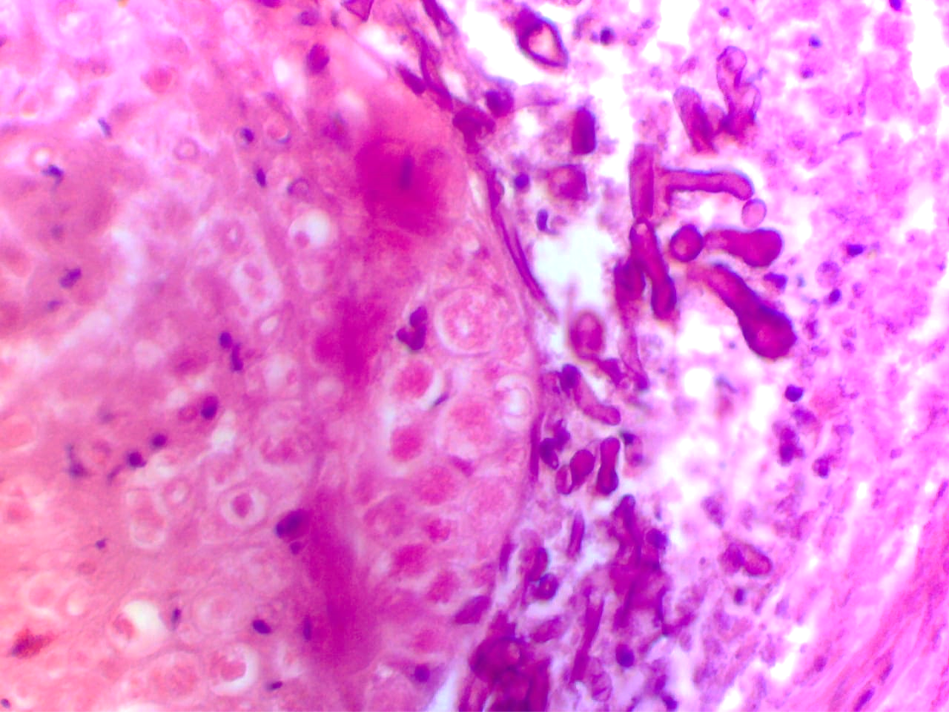
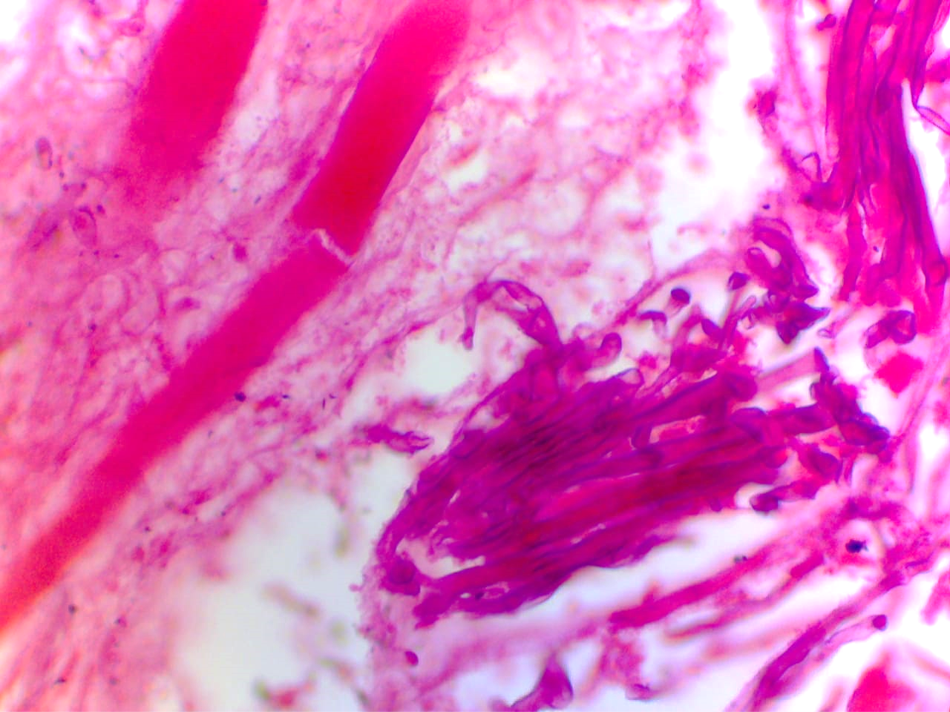
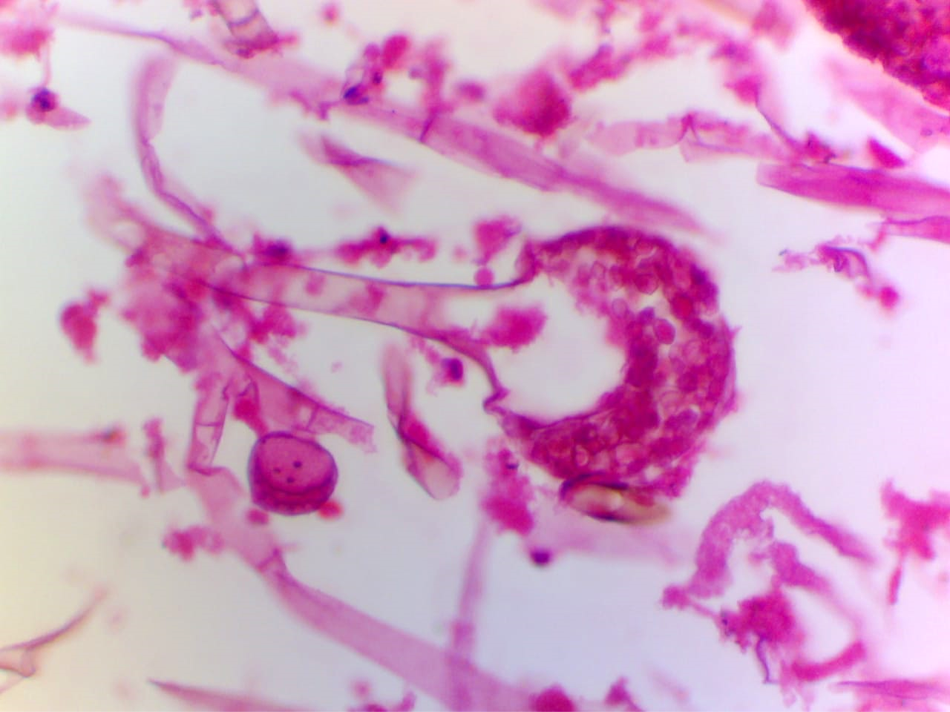
Histopathological examination showed tissue invasion by fungal hyphae, spores with characteristics of Mucormycosis in all patients. Fibrosis, chronic inflammatory infiltrate composed of eosinophils, lymphocytes, and plasma cells was noted in all cases. Granulomatous reaction with langhans and foreign body type of giant cells was noted in around 20 cases. Mucor was identified by the presence of much large and small flat, elongated non septate folded ribbon like fungal hyphae with obtuse angled branching patterns present throughout the inflamed rhino nasal tissue. These hyphae were seen specifically noted around blood vessels and nerves with features suggestive of fungal Anglo and neuro invasion. ([Figure 1], [Figure 2]) Muscle invasion and fat necrosis was observed in one case ([Figure 3]). Fungal osteomyelitis was also noted in twelve cases. Fungal balls and round to ovoid mature sporangia with column-shaped columella got noted as one of our astounded histopathological findings. ([Figure 4])
PAS and Grocott's Methenamine Silver staining further confirmed and highlighted the presence of many spores and hyphae of Mucor in inflamed rhino nasal tissue, indicative of heavy fungal load. KOH along with culture further established the diagnosis. After clinicopathologic correlation, a final diagnosis of rhino maxillary mucormycosis was established. Preserved fungal hyphae were not demonstrated in one of the case on routine stains. However, few ghost impressions of fungal hyphae could be appreciated on special stains. Most probably, this could be as a result of ongoing antifungal treatment. Two cases revealed mixed fungal infection with Mucor and Aspergillus both.
All these cases were observed mainly in second wave of COVID 19. Now in so called third wave, only flu like symptoms are there. Only rare cases are presenting with mild respiratory distress. Till date no complications are observed.
Interestingly, on retrospective analysis of Mucormycosis reported in our department, we found only ten cases in last decade, from 2010 to 2020 (approximately 120 months) out of total 76,555 reported histopathological cases (0.013%) as compared to 31 mucormycosis cases out of total 352 received histopathological cases in just three months of our study! (5.96%). Once classified under rare fungal disease, mucormycosis is regrouped under emerging pathogen.
Discussion
Mucormycosis (also called as zygomycosis) is a grave, not so common fungal infection caused by fungi in the order Mucorales.[9] They are omnipresent in environment and can be found in soil and decaying vegetable matter. They produce spores which get airborne and enter the body through inhalation or ingestion of fomites contaminated with spores. Thus, sporangiospores are the infective forms which give rise to the Angioinvasive hyphae in the human host, resulting in fulminant infections affecting various systems, including GIT, even in immunocompetent individuals.
It has recently emerged has devastating fungal infection worldwide, with variable clinical manifestations with risk factors including suppressed immunity, uncontrolled diabetes, iron overload and major trauma.[9] Poorly controlled diabetic patients are at high risk for acquiring Mucor infection due to defective innate immunity which impairs the phagocytic ability of neutrophils to kill fungal pathogens. In these patients sinus was found to be most affected area than pulmonary area.[10]
Infection initiates in nasal cavity and extends to paranasal sinuses. Most common site is middle turbinate, middle meatus and septum. It gets implanted and grows in the nasal cavity and sinuses. Early implantation of fungi is common in maxillary sinus with a mass of fungal growth called a fungal ball. The damp environment of the nose and paranasal sinuses supports the growth and invasion of fungi. Invasion of mucosa and bone depends upon the duration, host immunity, and severity of the disease. Bony infiltration is common in undiagnosed or untreated cases. Through bony erosion or angioinvasion, it may progress to brain through ethmoid sinuses or orbital apex.
In a prospective study conducted by Bala K et al. of 38 patients diagnosed with mucormycosis, the mean age was 40.3 years, and disease was more common in males (72%) as compared to females (28%).[11] Similar study by Roden et al. of 929 patients diagnosed with mucormycosis, the mean age was 38.8 years, and disease was more common in males (65%) as compared to females (35%).[12] In the present study the mean age was 56 years and the disease was more common in males (72%) as compared to females (28%).
Diabetic ketoacidosis, severe burns, steroid therapy, solid organ transplantation, prolonged corticosteroid therapy, hemochromatosis, patients with HIV, neutropenia, malnutrition, hematologic malignancies, have been shown to have frequent association with mucormycosis. However, 9% cases have been found to occur without any predisposing factors.[13]
Upward trend of invasive zygomycosis was already noted in patients with uncontrolled diabetes mellitus in India in studies conducted decade before.[14] Diabetes was the most common underlying condition (47.9%) in a study from Iran whereas studies from Greece, France and United States have revealed hematological malignancies as a leading risk factor.[15] Komur S et al reported that most common initial symptoms were fever, cellulitis, and facial pain whereas key predisposing factors were hematologic malignancies (52.9%), diabetes mellitus (25.5%), and solid malignancies (5.8%).[16] Rhino-Orbito-Cerebral Mucormycosis most common form and it is often seen in patients with diabetic ketoacidosis or with uncontrolled diabetes mellitus.[17] In our study, diabetes mellitus (90%) remains the most common risk factor.
Based on clinical features, It is classified as cutaneous, gastrointestinal, pulmonary and disseminated forms. Various morphological features have been described in historical literature like sporangiophores, rhizoid like structures and hyphae.[18]
Histopathological analysis in various studies have revealed invasion of blood vessels by hyphae, vasculitis with thrombosis, and tissue infarction. Chronic Granulomatous invasive fungal sinusitis has been noted in studies from Nigeria and Sudan.[19], [20] In our study histopathologic examination showed tissue invasion by fungal hyphae, spores with characteristics of Mucormycosis. Fibrosis, chronic inflammatory infiltrate, angio and neuro invasion, muscle invasion and fat necrosis was also noted. Three cases with granulomatous reaction were noted in our study. Mucor was identified throughout the inflamed rhino nasal tissue. Cases showing round to ovoid mature sporangia with column-shaped columella under microscope insinuate how a human body acts as a culture media exhibiting diversity of a human makeup. Our study involves the patient with caecal mucormycosis. Studied literature documents gastrointestinal mucormycosis as uncommon, Stomach being the most common affected site. In such cases, diagnosis is delayed, and the mortality rate is as high as 85%. Only 25% of gastrointestinal mucormycosis cases are diagnosed antemortem.[21]
To best of our knowledge, available Indian literature regarding mucormycosis did not reveal involvement of cartilage and skeletal muscle. However, some cases are reported outside India.[22]
Triple COVID wave has left healthcare workers encumbered and overwhelmed but management of mucormycosis in post COVID second wave was really challenging for medical professionals. But due to the increased awareness and advances in diagnostic techniques, many patients were managed efficiently.
Although fungal culture is considered as gold standard in establishing the diagnosis, observing Mucor like hyphae in involved tissues and direct examination play important role in diagnosis. Newer diagnostic modalities such as molecular based methods and detection of DNA of Mucorales in blood have also emerged now a days.[23] Diagnosis of mucormycosis is very gruel some and more difficult than other fungal infections as under normal laboratory conditions, there might be failure in sporulation process and culture results from the biopsies are often negative due to unviable organism in necrotic tissues.[24]
Source of Funding
None.
Conflict of Interest
None.
References
- HA Rothan, SN Byrareddy. The epidemiology and pathogenesis of coronavirus disease outbreak. J Autoimmun 2020. [Google Scholar]
- JAC Sterne, S Murthy, JV Diaz, AS Slutsky, J Villar, DC Angus. Association between administration of systemic corticosteroids and mortality among critically Ill patients with COVID-19 a meta-analysis. JAMA 2020. [Google Scholar]
- G Kumar, A Adams, M Hererra, ER Rojas, V Singh, A Sakhuja. Predictors and outcomes of hais in COVID-19 patients. Int J Infect Dis 2020. [Google Scholar]
- LM Kimmig, D Wu, M Gold, NN Pettit, D Pitrak, J Mueller. IL-6 inhibition in critically Ill COVID-19 patients is associated with increased secondary infections. Front Med (Lausanne) 2020. [Google Scholar] [Crossref]
- J Liu, S Li, J Liu, B Liang, X Wang, H Wang. Longitudinal characteristics of lymphocyte responses and cytokine profles in the peripheral blood of SARSCoV-2 infected patients. EBioMedicine 2020. [Google Scholar] [Crossref]
- . International Diabetes Federation. 2022. [Google Scholar]
- B Spellberg, J Edwards, A Ibrahim. Novel perspectives on mucormycosis: pathophysiology, presentation, and management. Clin Microbiol Rev 2005. [Google Scholar]
- AS Ibrahim, B Spellberg, TJ Walsh, DP Kontoyiannis. Pathogenesis of mucormycosis. Clin Infect Dis 2012. [Google Scholar]
- U Binder, E Maurer, C Lass-Flörl. Mucormycosis--from the pathogens to the disease. Clin Microbiol Infect 2014. [Google Scholar]
- I Mahalaxmi, K Jayaramayya, D Venkatesan, MD Subramaniam, K Renu, P Vijayakumar. Mucormycosis: An opportunistic pathogen during COVID-19. Environ Res 2021. [Google Scholar] [Crossref]
- K Bala, J Chander, U Handa, RS Punia, AK Attri. Rajpal Singh Punia, Ashok Kumar Attri, A prospective study of mucormycosis in north India: Experience from a tertiary care hospital. Med Mycol 2015. [Google Scholar]
- MM Roden, TE Zaoutis, WL Buchanan, TA Knudsen, TA Sarkisova, RL Schaufele. Epidemiology and outcome of zygomycosis: A review of 929 reported cases. Clin Infect Dis 2005. [Google Scholar]
- J Bhandari, PK Thada, S Nagalli. . Rhinocerebral Mucormycosis. StatPearls [Internet] 2021. [Google Scholar]
- A Chakrabarti, A Das, J Mandal, MR Shivaprakash, VK George, B Tarai. The rising trend of invasive zygomycosis in patients with uncontrolled diabetes mellitus. Med Mycol 2006. [Google Scholar]
- DE Corzo-León, LD Chora-Hernández, AP Rodríguez-Zulueta, TJ Walsh. Diabetes mellitus as the major risk factor for mucormycosis in Mexico: Epidemiology, diagnosis, and outcomes of reported cases. Med Mycol 2018. [Google Scholar]
- S Kömür, A S İnal, B Kurtaran, A Ulu, A Uğuz, HS Aksu. Mucormycosis: a 10-year experience at a tertiary care center in Turkey. Turk J Med Sci 2016. [Google Scholar]
- W Jeong, C Keighley, R Wolfe, WL Lee, MA Slavin, DCM Kong. The epidemiology and clinical manifestations of mucormycosis: A systematic review and meta-analysis of case reports. Clin Microbiol Infect 2019. [Google Scholar]
- A Skiada, I Pavleas, M Drogari-Apiranthitou. Epidemiology and Diagnosis of Mucormycosis: An Update. J Fungi (Basel) 2020. [Google Scholar]
- RD Deshazo. Syndromes of invasive fungal sinusitis. Med Mycol 2009. [Google Scholar]
- CN Asoegwu, RO Oladele, OO Kanu, CC Nwawolo. Chronic granulomatous invasive fungal rhinosinusitis in Nigeria: challenges of management. Int J Otorhinolaryngol Head Neck Surg 2020. [Google Scholar] [Crossref]
- G Petrikkos, A Skiada, O Lortholary, E Roilides, TJ Walsh, DP Kontoyiannis. Epidemiology and clinical manifestations of mucormycosis. Clin Infect Dis 2012. [Google Scholar]
- M Fadhel, S V Patel, E Liu. Disseminated Pulmonary with Isolated Muscular Mucormycosis in an Acute Myeloid Leukemia Patient: A Case Report and Literature Review. Am J Case Rep 2019. [Google Scholar]
- A Skiada, I Pavleas, M Drogari-Apiranthitou. Epidemiology and Diagnosis of Mucormycosis: An Update. J Fungi (Basel) 2020. [Google Scholar]
- P Badiee, A Arastefar, H Jafarian. Comparison of histopathological analysis, culture and polymerase chain reaction assays to detect mucormycosis in biopsy and blood specimens. Iran J Microbiol 2013. [Google Scholar]
