- Visibility 65 Views
- Downloads 12 Downloads
- DOI 10.18231/j.ijpo.2020.128
-
CrossMark
- Citation
Micro-invasive squamous cell carcinoma of gastro-esophageal junction in a teenage female: A rare case report
- Author Details:
-
Kafil Akhtar *
-
Mohd Talha
-
Sadaf Haiyat
-
Habeeb Raza
Introduction
Squamous cell carcinoma (SCC) of esophagus particularly of GE junction in older age group has been reported in the past. Post 1970’s many literatures report SCC in both younger and older age group owing to aggressive use of endoscopy and detection of H. pylori bacteria with special stain.[1] Its prognosis in younger age group remain controversial. Some case series report better prognosis while others report poor prognosis of SCC in younger age group when compared with older age group.[2], [3] Esophageal SCC occur worldwide with variable geographic distribution. Higher incidence of cases are seen in China, Iran, South Africa, France and Italy.[3]
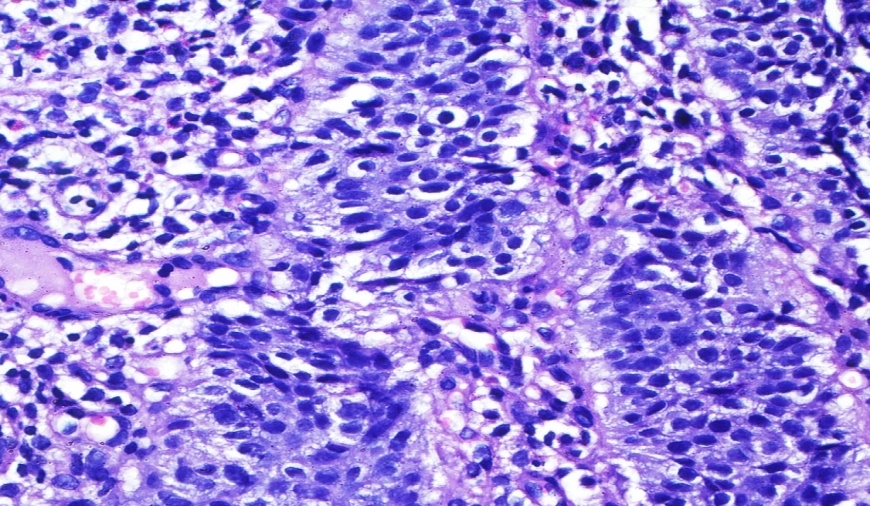
Microscpically, esophageal SCC show presence of atypical cell with nuclear hyperchromasia, clumped chromatin and loss of polarity of cells. Clinically, they present as fungative, ulcerative or infilterative lesions, ranging from well differentiated lesions with focal keratinization to poorly differentiated lesions showing marked cytologic atypia, increased mitotic activity (>!0 mitosis/ 10HPF) and widespread necrosis. Majority of cases present with metastasis to distant site with poor prognosis.[3]
Case Summary
A 15 years old teenage female presented to the surgery out-patient department with complaints of dysphagia since last 5 month initially for solid foods which progressively increased to liquids since last 2 month. She also complained of weight loss of approximately 8kgs during this period andepigastric pain associated with heartburn since the last 2 months. The pain was intermittent, dull in nature and occured shortly after food intake. However there was no complaint of pain during deglutition, chest pain or vomiting. There is no history of addiction or family history of upper GI malignancies.
On general examination, the patient was of thin built with wasting of muscles of extremities, afebrile, had low blood pressure of systolic 90/diastolic 50, raised pulse rate of 120 per minutes and pallor. Systemic examination was unremarkable except for presence of systolic murmur. Routine lab examinations like haemogram, general blood pictures, urine examination, liver function test, renal function test, lipid profile, iron profile, Vit. B12 assay and electrocardiogram were normal except for the presence of dimorphic (mixed nutritional deficiency) anaemia and low blood sugar (60mg/dl).
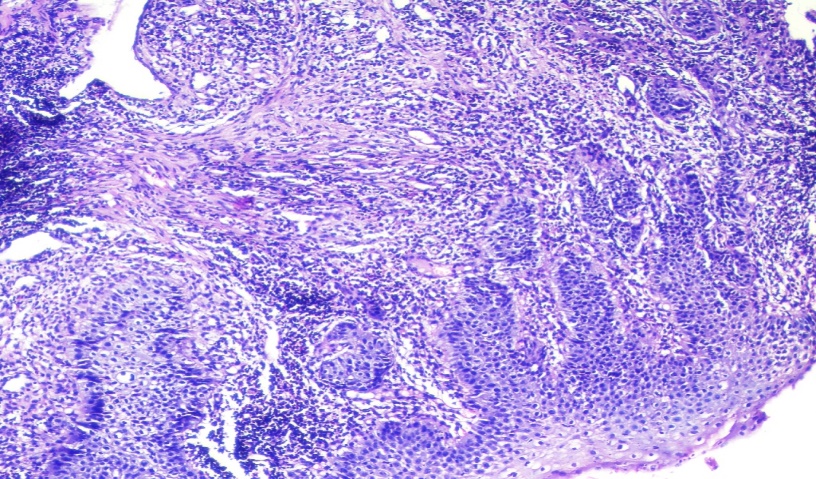
Imaging study viz., x ray of abdomen and chest showed normal studies. Barium swallow show rat tail appearance of lower third of the esophagus. Endoscopic examination showed ulcerated exophytic growth at GE junction partially obstructing the lumen and reddened area in stomach along greater curvature. Histopathology of GE junction growth showed marked dysplastic and koilocytic changes in stratified squamous lining. Superficial stroma showed nests of dysplastic squamous cells and reactive desmoplasia with moderate lymphocytic inflammation, findings consistent with microinvasive squamous cell carcinoma ([Figure 1], [Figure 2]). Staining of biopsy sections for H. pylori and Human papilloma virus (HPV) were negative. Sections from gastric biopsy was consistent with chronic atrophic gastritis. CT scan & MRI of abdomen and thorax did not show any evidence of metastasis. Patient underwent resection of GE junction with clearing of margins through left thoraco-abdominal approach along with end to end anastmosis. No lymph nodes were found to be enlarged intraoperatively. Patient was administered 50 Gy in 35 fractions of Co-60 radiotherapy for any residual tumour along with gradual resumption of oral diet. Our patient is doing well after 3 months of follow up.
Discussion
Squamous cell carcinoma of esophagus is among top 10th most common malignancies in the world. Adenocarcinoma of distal esophagus is relatively rare. However in past 25 years, incidence of esophageal adenocarcinoma has exceeded incidence of squamous cell carcinoma in the US and other western countries.[4], [5] Gastro-esophageal SCC is more common in black males. Male to female ratio is 7:1.5 years. Survival rate is 11% with no difference between various histologic types.[2] Risk factors include smoking, alcohol use, high salt intake in diet (pickles, fish), low fibre diet, poor socioeconomic status and H. pylori associated infection.[6], [7] Other risk factors include deficiency of vitamins A, C & E, occupational exposures to asbestos, perchloroethylene, combustion products, ionizing radiation and Human papilloma virus (HPV).[6]
Few cases of GE junction esophageal carcinoma have been reported so far. Youngest patient of esophageal carcinoma reported in India is a 8 year old girl with carcinoma in middle third portion with lung metastasis.[8] The prevalence of esophageal carcinoma is high in first degree relative with esophagitis. Tylosis, achalasia, esophageal diverticula, stricture and plummer–vinson syndrome are considered as premalignant conditions to esophageal carcinoma.
Microinvasive SCC is considered by some pathologists as early stage SCC with invasion of rete process in deeper tissues.[9] Few literature defined microinvasive SCC as histological subtype of SCC with irregular infiltrative border along with reactive desmoplasia and lymphocytic inflammation of deeper tissues.[9], [10] Microinvasive SCC has greater propensity for lymphatic and vascular channel infiltration. However owing to subjective variation in diagnosis of microinvasive SCC among pathologists, concrete literature comparing clinicopathological and prognostic differences between SCC and microinvasive SCC are lacking.[11], [12] However, many authors discuss poor prognosis of SCC in young compared to adults and emphasised careful monitoring and assessment of young patient with suspicion of esophageal SCC.[8], [13]
The differential diagnosis to be considered in case of GE junction SCC are achalasia, oesophageal stricture and benign esophageal tumour, especially leiomyoma. All these can be confirmed by combination of imaging studies (barium study, CT scan etc) and endocopic imaging biopsy of any mass lesion.
Treatment of disease depends on the stage of tumour at time of presentation. Surgery alone or in combination with radiotherapy are the treatment of choice. Surprisingly outcome of disease is independent of age of the patient.[13]
Conclusions
This case report emphasises the importance of considering squamous cell carcinoma in patients with complaint of dysphagia even at an early age and in the absence of any associated risk factors.
Source of Funding
None.
Conflict of Interest
None.
References
- D J Bowrey, G W B Clark, B I Rees, G T Williams, P D Carey. Outcome of oesophagogastric carcinoma in young patients. Postgrad Med J 1999. [Google Scholar]
- K Crew, A I Neugut. Epidemiology of upper gastrointestinal malignancies. Semin Oncol 2004. [Google Scholar]
- G D Stoner, L S Wang. Chemoprevention of esophageal squamous cell carcinoma with berries. Nat Prod Cancer Prev Ther 2012. [Google Scholar]
- D M Parkin, P Pisani, J Ferlay. Estimates of the worldwide incidence of eighteen major cancers in 1985. Int J Cancer 1993. [Google Scholar]
- W J Blot, S S Devesa, R W Kneller, J F Fraumeni. Rising incidence of adenocarcinoma of the esophagus and gastric cardia. J Pathol 2017. [Google Scholar]
- K CREW. Epidemiology of upper gastrointestinal malignancies. Seminars in Oncology 2004. [Google Scholar] [Crossref]
- Z F Zhang, R C Kurtz, G P Yu, M Sun, N Gargon, M Karpehjr. Adenocarcinomas of the esophagus and gastric cardia: the role of diet. J Nutr Cancer 2017. [Google Scholar]
- N. K. Soni, P.Chatterji Bikaner. Carcinoma of the oesophagus in an eight-year-old child. J Laryngol Otol 1980. [Google Scholar]
- A A Shankar, S Gokul. The dilemma of microinvasion. Head Neck Oncol 2014. [Google Scholar]
- M Pentenero, R Navone, F Motta, R Marino, L Gassino, R Broccoletti. Clinical features of microinvasive stage I oral carcinoma. Oral Dis 2011. [Google Scholar]
- J A Woolgar, A Triantafyllon. Pitfalls and procedures in the histopathological diagnosis of oral and oropharyngeal SCC: A review of the role of pathology in prognosis. Oral Oncol 2009. [Google Scholar]
- A Cardesa, P J Slootweg. Benign and potentially malignant lesions of squamous epithelium. Pathology of Head and Neck 2006. [Google Scholar]
- N G Nagdeve, G N Sarve, J B Hedawoo. Squamous cell carcinoma of esophagus in a 15-year-old boy. J Indian Assoc Pediatr Surg 2010. [Google Scholar]
How to Cite This Article
Vancouver
Akhtar K, Talha M, Haiyat S, Raza H. Micro-invasive squamous cell carcinoma of gastro-esophageal junction in a teenage female: A rare case report [Internet]. Indian J Pathol Oncol. 2025 [cited 2025 Sep 04];7(4):654-656. Available from: https://doi.org/10.18231/j.ijpo.2020.128
APA
Akhtar, K., Talha, M., Haiyat, S., Raza, H. (2025). Micro-invasive squamous cell carcinoma of gastro-esophageal junction in a teenage female: A rare case report. Indian J Pathol Oncol, 7(4), 654-656. https://doi.org/10.18231/j.ijpo.2020.128
MLA
Akhtar, Kafil, Talha, Mohd, Haiyat, Sadaf, Raza, Habeeb. "Micro-invasive squamous cell carcinoma of gastro-esophageal junction in a teenage female: A rare case report." Indian J Pathol Oncol, vol. 7, no. 4, 2025, pp. 654-656. https://doi.org/10.18231/j.ijpo.2020.128
Chicago
Akhtar, K., Talha, M., Haiyat, S., Raza, H.. "Micro-invasive squamous cell carcinoma of gastro-esophageal junction in a teenage female: A rare case report." Indian J Pathol Oncol 7, no. 4 (2025): 654-656. https://doi.org/10.18231/j.ijpo.2020.128
