- Visibility 259 Views
- Downloads 38 Downloads
- Permissions
- DOI 10.18231/j.ijpo.2020.077
-
CrossMark
- Citation
Histopathological spectrum of lesions in gastrointestinal endoscopic biopsy: A prospective study of 500 cases
- Author Details:
-
Saurabh Sharma
-
Kavita Kumari *
-
Satyendra Sharad
-
Garima Shah
-
Neelam
Abstract
Introduction: Lesion of the gastrointestinal tract is a very common condition encountered in medical science. An endoscopic biopsy is a favourable tool for early diagnosis and management of these conditions. The aim of the work is to study the histopathological spectrum of gastrointestinal endoscopic biopsy.
Materials and Methods: In a prospective study of 500 biopsies, Formalin-fixed tissue was processed and stained with Hematoxylin-Eosin stain and studied under the microscope.
Result: A wide spectrum of neoplastic and non-neoplastic lesions was noted with male preponderance in most of the gastrointestinal tract. The commonest age group was 6th decades of life. Mean age being 51.83years. Predominant sample collected was from stomach accounting for 36.6% of total gastrointestinal biopsies. The ratio between non-malignant: malignant lesion was 2.7:1. Majority of the malignancy was Adenocarcinoma seen in 71 out of 135 cases closely followed by Squamous cell carcinoma (62/135). Most of the oesophageal malignancy was squamous cell carcinoma whereas adenocarcinoma was common in rest of the gastrointestinal tract. Gastritis was the commonest non-neoplastic lesion. Celiac disease was common in our study. Eight cases of adenomatous polyp identified, four of them showed high-grade dysplasia.
Conclusion: Celiac disease and inflammatory bowel disease need further studies as there were many overlapping features which make a definitive diagnosis difficult. Endoscopy itself is insufficient in the diagnosis and management of gastrointestinal tract disease and biopsy must be performed in all cases of suspected endoscopic finding. Conditions like Barrett’s oesophagus, Celiac disease, Inflammatory Bowel Disease and high-grade dysplasia needs timely intervention to avoid more serious complications.
Introduction
Disorder of gastrointestinal tract is one of the most commonly encountered problems in clinical practice. A high degree of mortality and morbidity is caused by them.[1] Lesions of the gastrointestinal tract include neoplastic and non-neoplastic lesions like infections, inflammation, vascular disorders, physical and toxic injury etc.[2] The upper gastrointestinal flexible fibre optic endoscopy was first used in 1968 and proved to be a major breakthrough in the diagnosis of gastrointestinal tract lesions. Endoscopic biopsy is a convenient procedure and no major surgery is required. Reaching the inaccessible sites in the gastrointestinal tract is facilitated by the use of an endoscope or colonoscope which helps in direct visualizing the lesion and taking of biopsy from the suspicious site. An endoscopic or colonoscopy biopsy for histopathologic examination is not only used to diagnose malignant and inflammatory lesions but also for monitoring the course, the extent of disease, response of the therapy and early detection of complications.[3] It forms a large proportion of the specimens that are analyzed in the pathology department and considered as the current gold standard for accurate assessment of patients with symptoms of Gastrointestinal tract disease.
Aims and Objectives
To determine the spectrum of histopathological lesions of the gastrointestinal tract.
To determine the frequency of the lesion among different age group and sex.
Materials and Methods
A prospective study was carried out in the Department of Pathology Dr. R.P.G.M.C at Tanda for a period of 1 and ½ years from January 2018 to May 2019 with 500 GIT endoscopic biopsies received in the pathology department. Histopathologic spectrum and its frequency were studied.
Inclusion criteria
All gastrointestinal tract endoscopic biopsies of all age and sex.
Exclusion criteria
Inadequate biopsies.
Resection specimen.
Liver and gall bladder specimen.
These filter paper mounted biopsies were received in the properly labelled and tightly closed container containing 10% formalin. Which was then examined grossly for the number and appearance. After fixation biopsy was processed and embedded in paraffin with orienting the specimen mucosal surface uppermost. Three to four micron thick sections were cut perpendicular to this surface. Sections were stained with routine Hematoxylin and Eosin stain (H and E) and mounted with coverslips using Distyrene Plasticizer Xylene (DPX) as mountant. Additional sections were stained with Giemsa to observe H. Pylori and Periodic Acid Schiff (PAS) stain were performed wherever necessary. Analysis of the spectrum of the lesion as done. For celiac disease Modified Marsh classification[4] was done on duodenal biopsies.[5] All tumours were classified according to WHO classification.
Result
In the present study, 500 GI biopsy sample was studied. Out of five hundred patients, 211 were female and 289 were male. The youngest patient was 4 years male child with a juvenile polyp and the oldest was 95 years old male with an adenomatous polyp. Both youngest (15 years) and oldest female patient (91 years) were having non-specific Duodenitis. The commonest age group presented with gastrointestinal complaint were in their 6th decades of life. Mean age being 51.83years. Among 500 biopsies 81 (16.2%) were esophageal, 183 (36.6%) gastric, 119 (23.8%) were duodenal and 117(23.4%) colorectal biopsies. ([Table 1])
Oesophagal biopsy
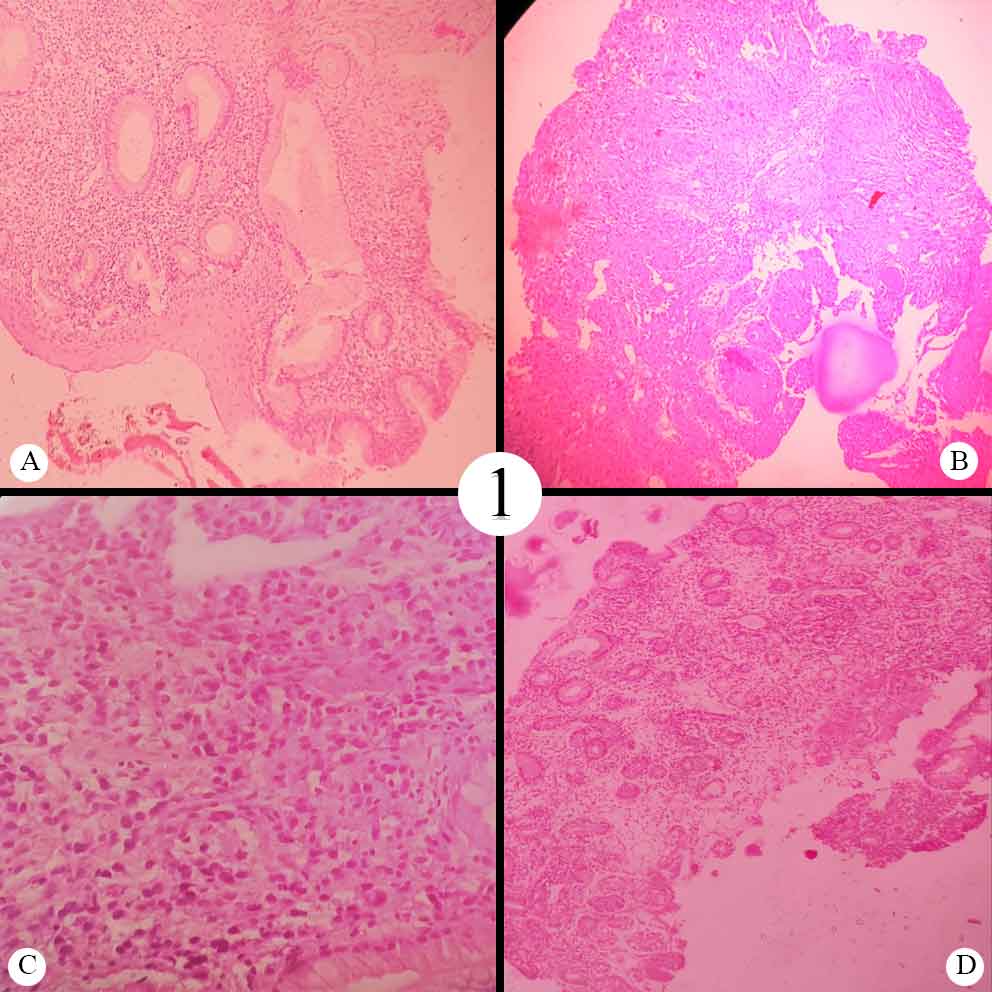
Maximum no of oesophageal biopsy cases was in their 7th decades of life. Male: Female ratio was 1.89:1. Neoplastic lesions (76.5%) outnumbered the non-neoplastic conditions (23.5%) making a 3.26:1 ratio. Among the neoplastic lesions squamous cell carcinoma was the most prevalent lesion forming 98.41%. Poorly differentiated adenocarcinoma accounting for 1.58%. Majority of squamous cell carcinoma were moderately differentiated. The youngest patient with squamous cell carcinoma was a female of 28years. The most common age group involved was 6th decades of life. Mean age of malignant oesophagal tumour was 52 years. The second most common lesion was esophagitis accounting for 11.11% cases. Three of eighty-one biopsies were sent with clinical suspicion of Barrett’s oesophagus on endoscopy. Microscopic examination showed gastric type mucosa with and without intestinal metaplasia. Dysplastic squamous cell lining was seen in 3 of the biopsies. ([Table 2] A)([Figure 1] A, B, C)
Gastric biopsy
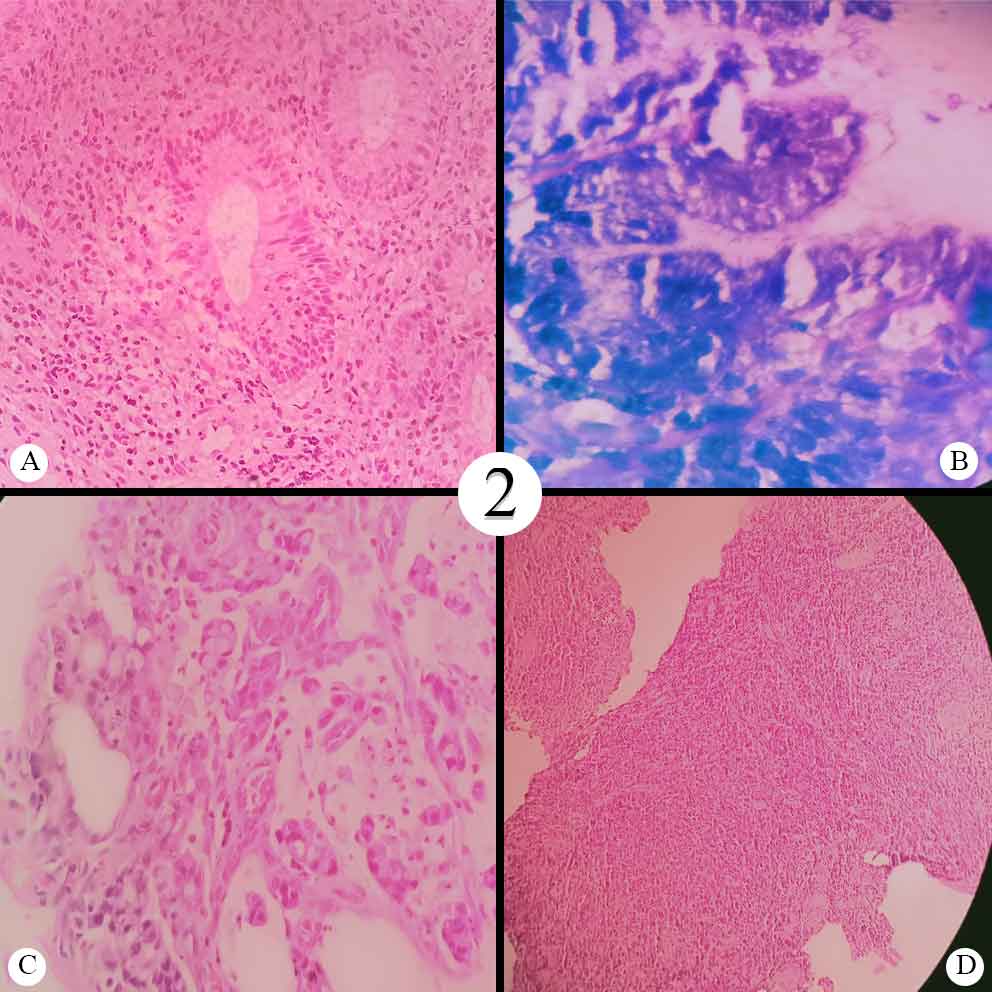
The most common endoscopic biopsy was gastric biopsy accounting for 183 out of 500 cases (36.6%) and the most common age group was 51 to 60 years, accounting for 24.04%. Male: female ratio was 1.54:1. The youngest patient was 9 years old male child shows histopathologic features of Helicobacter Pylori(H.Pylori) associated with chronic gastritis. Six of 183 cases (3.3%) were within normal histologic limits which included the 90 years old female patients also. Out of 183 gastric biopsies, 139(75.9%) cases were non- neoplastic and 38(20.7%) cases were neoplastic. Most common malignancy was moderately differentiated adenocarcinoma. Six out of 34 cases (17.64%) cases show histopathologic features of signet ring adenocarcinoma. Two cases showed a dense monomorphic population of lymphoid cells infiltrating the entire biopsy tissue. The native tissue was barely visible in the biopsy submitted for the examination. Diagnosed with lymphoma was offered. Among 139 cases of non-neoplastic lesion 136 shows histopathologic features of gastritis. On microscopic examination, 3.67% of cases show gastric mucosa infiltration by neutrophil resulting in the diagnosis of acute gastritis. Chronic gastritis was seen in 81.61% biopsies having plasma cell, lymphocytes infiltrating gastric mucosa. Nineteen cases (13.97%) showed features of chronic active gastritis. H. pylori infection was seen in 52.20% of cases. Which is confirmed by Giemsa stain as curvilinear bacteria. One case of atrophic gastritis was also seen. There were features of chronic gastritis along with glandular atrophy. ([Table 2] B) ([Figure 1]D, [Figure 2] A,B,C,D)
Duodenal biopsy
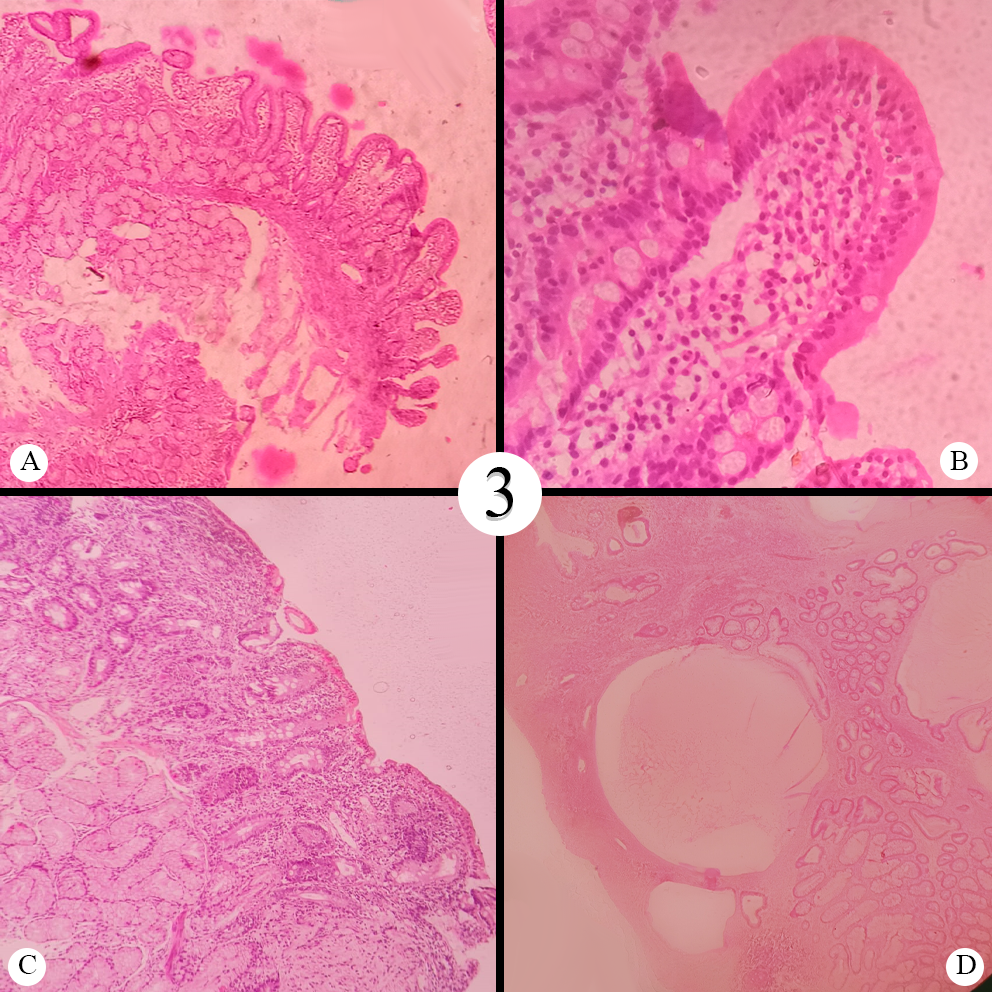
Among 119 cases of duodenum biopsies, all were non-neoplastic. Male: Female ratio was 0.72:1. Commonest age group involved was 4th decades. The youngest patient was 11 years male and the oldest patient was 91 years female were having Chronic Non-Specific Duodenitis as majority of the cases (58.82%). The microscopic exam showed increased intraepithelial lymphocytes(IEL), plasma cell infiltrates and oedema in lamina propria. In 35cases (29.41%) duodenum biopsy was submitted with a clinical impression of malabsorption syndrome and to rule out celiac disease(CD). Anti-transglutaminase antibodies were done in only 12 of the patients. All were having either villous changes, scalloping of the duodenal mucosa on endoscopy or strong clinical suspicion. Rest 23 cases of suspected celiac disease were either serologically negative or Anti-Transglutaminase Antibodies level not done. Fifteen out of thirty-five cases showed only increased intraepithelial lymphocytes more than 30/100enterocytes with mild oedema in lamina propria falling in Modified Marsh grade 1 celiac disease. Seven cases showed increased IEL >30/100 enterocytes and mild to moderate crypt hyperplasia histopathologically graded as Modified Marsh grade 2 celiac disease. Additional villous atrophy was noted in 13 of the cases. Three with total villous atrophy (Modified Marsh grade 3c). Subtotal (grade 3b) and partial villous atrophy (grade 3a) were seen in four and six cases respectively. Among those with increase Anti-transglutaminase antibodies level three were of grade 3c, four and two of 3a and 3b respectively, two of grade 2 and one case of grade 1. Around 10% of biopsies showed normal histology of duodenum. Dysplasia and ulcer were observed in one case each.([Table 3] A) ([Figure 3] A,B,C)
Colorectal biopsy
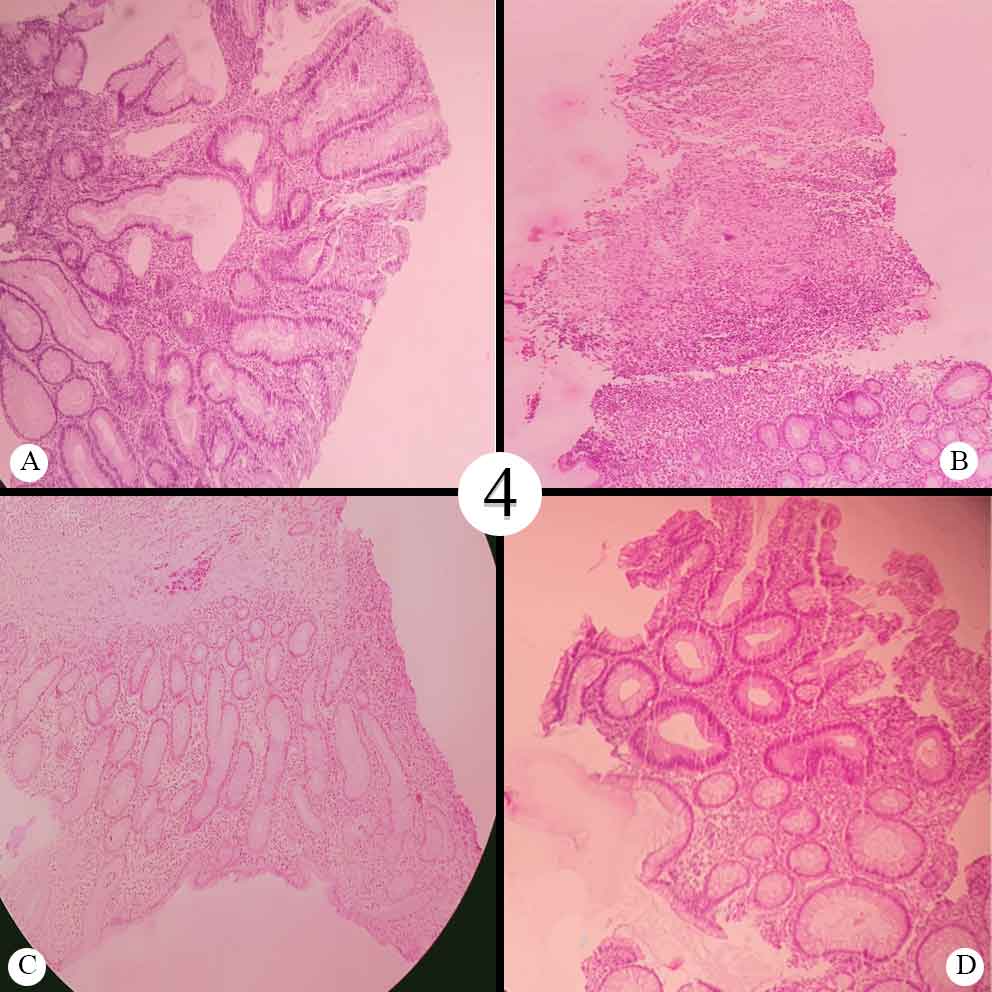
Among all the colonic biopsies, histologically 65 cases (55.55%) were diagnosed as non-neoplastic lesions and 43 cases (36.75%) were diagnosed as neoplastic lesions. The sixth decade was the commonest age group involved. Mean age being 50.72 years. The youngest patient was four years old male with a juvenile polyp. Microscopic examination showed cystically dilated glands filled with inspissated inflammatory debris in an edematous lamina propria. There was inflammatory cell infiltrate in lamina propria. The oldest patient was 95 years old male with an adenomatous polyp. Nine out of 117 cases (7.69%) were within normal histological limits. Among the non-neoplastic lesion colitis was the commonest lesion (24.78%) followed by inflammatory bowel disease(IBD) accounting for 17.09% of cases. Seventeen of 20 cases of IBD cases (85%) diagnosed as ulcerative colitis. There was evidence of cryptitis, crypt abscess, crypt distortion, basal plasmacytosis and mixed inflammatory cell infiltrate in lamina propria. Three of IBD cases showed non-caseating granulomas and transmural lymphoplasmacytic infiltrate and were signed out as Crohn's disease. Other non-neoplastic polyps four cases of the juvenile polyp, two Hyperplastic polyp characterized by elongated glands and crypts without serrated appearance. Six cases of inflammatory polyp having focal mucosal erosions and inflammatory cells infiltration in lamina propria seen.
Among 43 neoplastic lesions, benign lesions were in seen in 12 cases (27.90%) and Malignant lesions were observed in 36 cases (83. 72%). One case showed dysplasia of high-grade in the glandular lining. Amid the benign lesion, 8 cases of adenomatous polyp all showed histopathologic features of tubular adenoma characterized by an increased number of tubular glands with nuclear stratification, hyperchromatic nuclei limited to the lower one-third of glandular epithelium. High-grade dysplasia was observed in 4 cases of an adenomatous polyp.
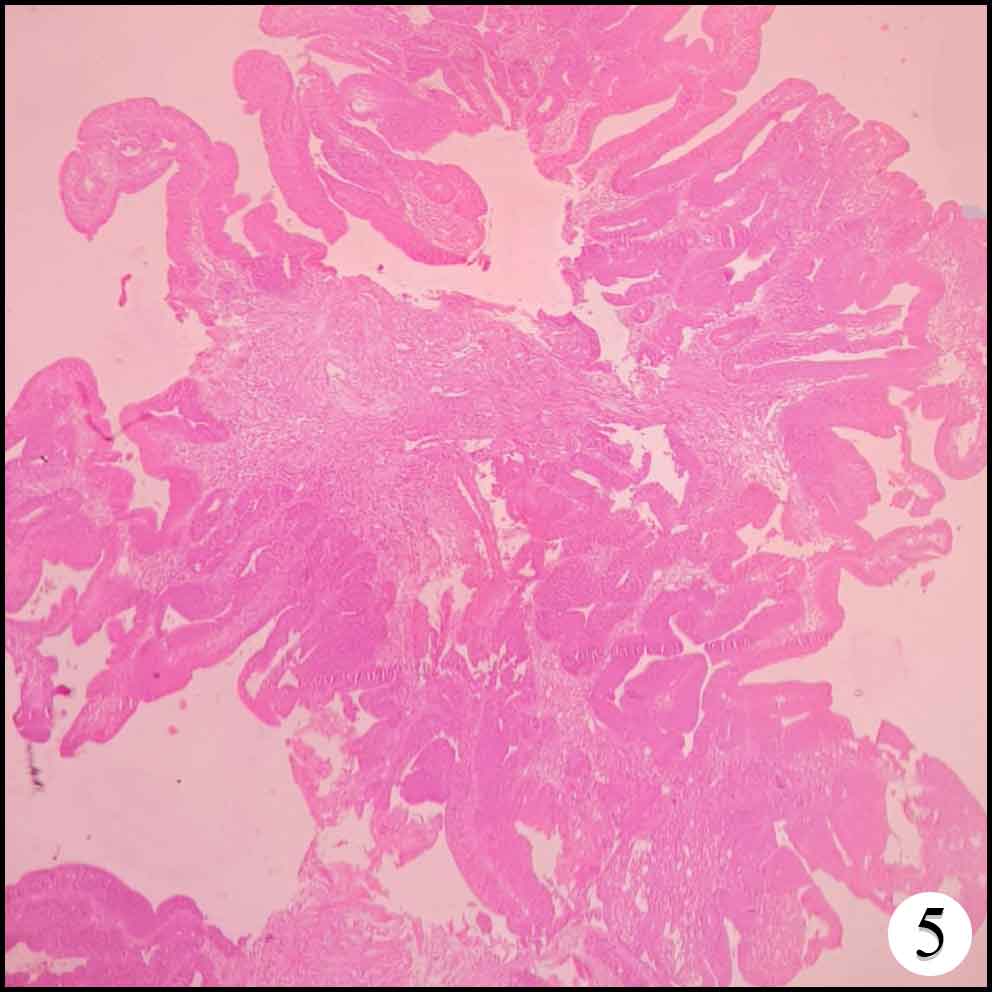
Thirty six cases of adenocarcinomas, commonest being moderately differentiated, identified which was characterized by malignant glands with poor outlines. Well-differentiated adenocarcinomas were seen in 9 biopsies, characterized by well-formed malignant glands with infiltration into the submucosa. Poorly differentiated carcinomas were observed in 6 cases, characterized by malignant cells in sheet, cords and groups with no glandular structures. Signet shaped malignant cells infiltrating into the submucosa was observed in one case. Mean age of malignancy was 51.62 years. ([Table 3] B) ([Figure 3]D, [Figure 4]A, B, C, D)
| Age range | Oesophagal biopsy | Gastric biopsy | Duodenal biopsy | Colonic biopsy |
| 0-10yrs | - | 1 | - | 2 |
| 11-20yrs | - | 3 | 11 | 3 |
| 21-30yrs | 2 | 18 | 22 | 11 |
| 31-40yrs | 5 | 31 | 25 | 20 |
| 41-50yrs | 4 | 26 | 22 | 23 |
| 51-60yrs | 22 | 44 | 18 | 28 |
| 61-70yrs | 25 | 29 | 13 | 14 |
| 71-80yrs | 16 | 19 | 5 | 7 |
| 81-90yrs | 7 | 12 | 2 | 8 |
| 91-100yrs | - | - | 1 | 1 |
| Total | 81 | 183 | 119 | 117 |
| Male: female | 1.89:1 | 1.54:1 | 0.72:1 | 1.78:1 |
| Site | Disease | No of cases | Percentage |
| (A) Oesophagus (n=81) | WNL | 3 | 3.7 |
| Esophagitis | 9 | 11.1 | |
| Barrett’s | 3 | 3.7 | |
| Dysplasia | 3 | 3.7 | |
| Squamous cell ca | 62 | 76.6 | |
| Adenocarcinoma PD | 1 | 1.2 | |
| (B) Gastric (n=183) | WNL | 6 | 3.28 |
| Gastritis | 136 | 74.32 | |
| a) Acute gastritis | 5 | 4.41* | |
| b) Chronic gastritis | 111 | 81.61* | |
| c) Chronic active gastritis | 19 | 13.97* | |
| d) Atrophic gastritis | 1 | 0.73* | |
| Dysplasia | 2 | 1.09 | |
| Polyp | 3 | 1.64 | |
| Adenocarcinoma | 34 | 18.58 | |
| Lymphoma | 2 | 1.09 |
| Site | Disease | No. of cases | Percentage |
| (A) Duodenal (n=119) | WNL | 12 | 10.08 |
| Nonspecific Duodenitis | 70 | 58.82 | |
| Suspected celiac | 35 | 29.41 | |
| Dysplasia | 1 | 0.84 | |
| Ulcer with Metaplasia | 1 | 0.84 | |
| (B) Colorectal (n=117) | WNL | 9 | 7.7 |
| Colitis | 20 | 17.09 | |
| IBD | 29 | 24.78 | |
| (a)Ulcerative colitis | 23 | 79.31* | |
| (b)Crohn’s | 6 | 20.68* | |
| Granulomatous lesion | 2 | 1.7 | |
| Dysplasia | 1 | 0.85 | |
| Polyp | 20 | 17.09 | |
| a) Non neoplastic | 12 | 60* | |
| b)Neoplastic | 8 | 40* | |
| Adenocarcinoma | 36 | 30.76 |
| Studies | % of biopsies | Neoplastic | Non-neoplastic | Commonest lesion |
| (A) Oesophageal biopsy | ||||
| Present study(n=500) | 16.2% | 77.7% | 22.3%. | Squamous cell ca 76.50% |
| Jaynul Islam et al (n=110) | 20% | 81.82% | 18.18% | Squamous cell ca 81.25% |
| Somani et al.(n==100) | 39% | 69.20% | 30.80% | Squamous cell ca 82.60% |
| (B) Gastric biopsy | ||||
| Present study (n=500) | 36.6% | 20.76%) | 75.9% | Gastritis(74.31%) |
| Hirachand et al(n=243) | 90% | 12.37% | 86.67% | Gastritis (78.99%) |
| Jaynul Islam et al (n=110) | 66.36% | 45.20% | 54.75% | Adenocarcinoma (45.20%) |
| Studies | % of biopsies | Neoplastic | Non-neoplastic | Commonest lesion |
| (A) Duodenal biopsy | ||||
| Present study(n=500) | 23.8% | No | 100% | Nonspecific Duodenitis(58.82%) |
| Hirachand et al(n=243) | 3.70% | No | 100% | Nonspecific Duodenitis(66.66%) |
| Jaynul Islam et al (n=110) | 13.64% | 13.33% | 86.66% | Hyperplastic polyp(73.33%) |
| Somani et al.(n=100) | 9% | No | 100% | Nonspecific Duodenitis(100%) |
| (B) Colorectal biopsy | ||||
| Present study (n=500) | 23.4% | 36.75% | 55.55% | Adenocarcinoma (30.76%) |
| Abilash et al(n=250) | 100% | 39.2% | 60.8% | Colitis 28.4% |
| Makaju R et al (n=95) | 100% | 24.21% | 60% | non-neoplastic polyps (32.63%) |
Discussion
Oesophagal biopsy
The present study is comparable with Somani et al.[6] and Jaynul Islam.[7] et al. In all the three studies the most common age group involved was 7th decades of life with a male predominance. In our study neoplastic lesions (77.7%) were more commonly encountered than non-neoplastic lesions (22. 3%). Squamous cell carcinoma was the most common among neoplastic lesion. Mean age of malignancy was 51.94years whereas Jaynul islam observed a mean age of 56.56 Years for the same. Oesophagitis was most common amongst non-neoplastic lesions making 11.11% (9 out of 19 cases). Barrett’s oesophagus was confirmed in 3.7% cases of. A similar finding was observed by Somani et al. who observed 6% of oesophagitis and 1% Barrett’s oesophagus. Jaynul Islam et al. found 18.18% of oesophagitis and no case of Barrett’s.([Table 4] A)
Gastric biopsy
In the current study, the most common biopsy submitted was gastric biopsy (36.6%) with a male-female ratio of 1.54:1, which was comparable to the study by Puvitha R Duraisamy et al[8] in which they received 34.69% gastric biopsy with male-female ratio 1.5:1. The most common age group undergoing gastric biopsy was 6th decades whereas it was 7th decades in Jaynul islam et al. study.Gastritis being commonest lesion and adenocarcinoma commonest malignancy(18.54%) in our and Hirachand et al. study(12.33%). Jaynul islam et al. observed adenocarcinoma as the commonest lesion (45. 20%). This disparity may be due to the small sample size of their study. Mean age of malignancy in the present study was 51.82 years in comparison to 60.12 years in Jaynul islam et al study. In the present study, H. pylori positivity was seen in 52.20% cases which is similar to Hirachand et al. (53.42%). These two studies showed a lesser percentage of H pylori positivity than the observed prevalence rate of 80% in India and other developed countries.[9] This can be attributed to the irrational use of proton pump inhibitors, Amoxycillin/clarithromycin, metronidazole before taking a biopsy for histopathology. ([Table 4] B)
Duodenal biopsy
In the present study mean age of patients with duodenal biopsy was 43.40 years and most common age group involved was 4th decades in comparison of 49.47 years and 5th decades in the study by Jaynul Islam et al. The youngest patient was 11 years old male and the oldest patient was 91 years old female. On Histopathologic examination of both showed features of Non-Specific Duodenitis as there was mild increases in intraepithelial lymphocytes and mild oedema in lamina propria. This observation was similar to a study conducted by Hirachand et al. out of 117 cases one case of the duodenal ulcer was noted whereas Hirachand et al. noted 2 cases of ulcers. Jaynul Islam et al. noted 13.33% of cases of malignancy all adenocarcinoma,73.33% cases of the hyperplastic polyp and no case of Duodenitis. These difference can be attributed to the larger sample size of the present case as well as different dietary habits of study groups. In the present study out of 35 (29.41%) suspected cases of celiac disease Anti-Transglutaminase was raised in twelve. Nine cases of them had modified marsh grade III disease. Manjusha Milind Karegar et al observed 28% cases of celiac disease with slight female preponderance.[10] The high proportion CD in the present study as compared to the prevalence rate of 1% in general population[11] can be attributed firstly to the fact that our study was conducted on the symptomatic patients and secondly to the overlapping features of other conditions like autoimmune enteropathy, tropical sprue and many other with increased IEL and/or villous atrophy and crypt hyperplasia that can mimic Celiac disease on biopsy. Regular follow up, mandatory anti transglutaminase antibodies estimation, repeat biopsy is required to filter out the overlapping conditions.([Table 5] A)
Colorectal biopsy
Colorectal biopsy comprised of 23.4% cases whereas in the comparison groups the study was focused on colonoscopic biopsy. There is male preponderance in all the studies. The mean age of patients of colonic biopsy 50.72yr with maximum cases of the patient was in their sixth decades of life (23.93%). Makaju et al observed mean age of 41.2 years, maximum cases were in the age group of 20-39 years (31.58%).[12] Percentage of neoplastic to non-neoplastic cases found to be similar to Abilash et al[13] and Makaju R et al. Our study observed that the commonest lesion was adenocarcinoma accounting for 30.76%, comparable to Abilash et al. who reported 21.6% cases of it. Whereas Makaju et al. observed only 11.58% of malignancy. The non-neoplastic polyp in the current study was 10.25%. The most common non-neoplastic lesion was colitis similar to Abilash et al but in discordance with Makaju R et al. They observed non-neoplastic polyps (32.63%) as the commonest lesion. In our study, inflammatory bowel disease was seen in 17.09% of cases with 85% of cases of ulcerative colitis and15% cases of Crohn's disease. These findings were in concordance with studies by Abilash et al. (26.97%). ([Table 5] B)
Conclusion
A variety of neoplastic and non- neoplastic lesions were observed in the present study across a wide range of site, age and sex distribution. Endoscopy of the gastrointestinal tract though is diagnostic, histopathology is the gold standard. It is advisable to correlate endoscopic and colonoscope findings with histopathological findings for the final clinical diagnosis of gastrointestinal tract disease. It aids the clinicians for early detection of lesions and further management.
Source of Funding
None.
Conflict of Interest
None.
References
- Hirachand S, Sthapit RR, Gurung P, Pradhanang S, Thapa R, Sedhai M. Histopathological spectrum of upper gastrointestinal endoscopic biopsies. J BP Koirala Inst Health Sci. 2018;1(1):67-74. [Google Scholar]
- Memon DF, Baloch DK, Memon DAA. Upper gastrointestinal endoscopic biopsy; morphological spectrum of lesions. Professional Med J. 2015;22(12):1574-9. [Google Scholar]
- Krishnappa R, Horakerappa MS, Ali K, Gouri M. A study on histopathological spectrum of upper gastrointestinal tract endoscopic biopsies. Int J Medical Res Health Sciences . 2013;2(3):418-24. [Google Scholar]
- Oberhuber G, Granditsch G, Vogelsang H. The histopathology of coeliac disease: time for a standardized report scheme for pathologists. Eur J Gastroenterol Hepatol. 1999;11:1185-94. [Google Scholar]
- Somani. Histopathological Study of The Upper Gastrointestinal Tract Endoscopic Biopsies. Ann Pathol Lab Med. 2018;5(8):684-8. [Google Scholar]
- Islam SMJ, Ahmed ASMM, Ahmad MSU, Hafiz S. Endoscopic and Histologic Diagnosis of Upper Gastrointestinal Lesions, Experience in a Port City of Bangladesh. Chattagram Maa-O-Shishu Hosp Med Coll J. 2014;13(3):11-4. [Google Scholar]
- Duraisamy PR, chithambram L, Ibrahim S, Madasamy K, Balan L, Thandavarayan P. Histomorphology Of Upper GI Endoscpic Biopsies: A Study In Urban Care Centre. Ann Appl Bio-Sci. 2017;4(4):A188-94. [Google Scholar]
- Dhakal M, Dhakal O. Prevalence of Helicobacter pylori infection & pattern of gastrointestinal involvement in patients undergoing upper gastrointestinal endoscopy in Sikkim. Indian J Med Res. 2018;147(5):517-20. [Google Scholar]
- Karegar MM, Kothari K, Mirjolkar AS. Duodenal biopsy in malabsorption-A clinicopathological study. Indian J Pathol Oncol. 2016;3(2):197-201. [Google Scholar]
- Mustalahti K, Catassi C, Reunanen A, Fabiani E, Heier M, McMillan S, et al. The prevalence of celiac disease in Europe: Results of a centralized, international mass screening project. Ann Med. 2010;42(8):587-95. [Google Scholar]
- Makaju R. Clinico-pathological correlation of colorectal diseases by colonoscopy and biopsy. Kathmandu Univ Med J. 2017;15(58):173-8. [Google Scholar]
- Chandrakumari AS, Singaravelu S. Histopathological Interpretation Of Colonic Mucosal Biopsies With Clinical Correlation: A Study In A Tertiary Care Hospital Kerala. Ann Pathol Lab Med. 2017;4(5):A565-72. [Google Scholar]
How to Cite This Article
Vancouver
Sharma S, Kumari K, Sharad S, Shah G, Neelam . Histopathological spectrum of lesions in gastrointestinal endoscopic biopsy: A prospective study of 500 cases [Internet]. Indian J Pathol Oncol. 2020 [cited 2025 Sep 28];7(3):284-291. Available from: https://doi.org/10.18231/j.ijpo.2020.077
APA
Sharma, S., Kumari, K., Sharad, S., Shah, G., Neelam, (2020). Histopathological spectrum of lesions in gastrointestinal endoscopic biopsy: A prospective study of 500 cases. Indian J Pathol Oncol, 7(3), 284-291. https://doi.org/10.18231/j.ijpo.2020.077
MLA
Sharma, Saurabh, Kumari, Kavita, Sharad, Satyendra, Shah, Garima, Neelam, . "Histopathological spectrum of lesions in gastrointestinal endoscopic biopsy: A prospective study of 500 cases." Indian J Pathol Oncol, vol. 7, no. 3, 2020, pp. 284-291. https://doi.org/10.18231/j.ijpo.2020.077
Chicago
Sharma, S., Kumari, K., Sharad, S., Shah, G., Neelam, . "Histopathological spectrum of lesions in gastrointestinal endoscopic biopsy: A prospective study of 500 cases." Indian J Pathol Oncol 7, no. 3 (2020): 284-291. https://doi.org/10.18231/j.ijpo.2020.077
