- Visibility 215 Views
- Downloads 35 Downloads
- DOI 10.18231/j.ijpo.2019.127
-
CrossMark
- Citation
Rare tumors of retroperitoneum-A diagnostic challenge
- Author Details:
-
Ranuva Vaishnavi
-
Bandavat Sankar Naik
-
P Premalatha
-
Ch Ramya
-
I V Renuka *
Introduction
Primary retroperitoneal neoplasms are rare comprising 0.1-0.2% of all malignancies.[1] In retroperitoneum malignant tumours are more frequent than benign lesions but elsewhere in the body benign diseases predominate. Soft tissue (mesenchymal) tumours of retroperitoneum are less common, but constitute 15% of all primary sarcomas.[2] Retroperitoneal tumours can cause a diagnostic dilemma and present several therapeutic challenges because of their rarity, relative late presentation and anatomical location often in close relationship with several vital structures in the retroperitoneal space.[3] We aim to study the distribution of both benign & malignant tumors of the retroperitoneum with emphasis on the clinicopathological picture of the rare tumors we encountered.
Materials and Methods
Biopsies of 62 retroperitoneal tumors from patients who were admitted to the hospital from January 2013 to December 2017 were studied. Complete clinical details including radiographic findings were procured. All specimens were fixed in 10% Formalin and then subjected to macroscopic examination. Representative samples were taken, processed and stained with routine Hematoxylin & Eosin stains. Special stains and IHC were used where ever necessary.
Results
A total of 62 retroperitoneal tumours were studied. Amongst the 62 cases, 5 cases were under the age of 14 years and 57 cases were above 14 years. Males were 33 cases & Females were 29 cases with a male is to female ratio being 1.1:1. Number of benign tumors in children were 1 case & in adults 18 cases. Total malignant tumors were 4 cases in children and in adults 39 cases.[Table 1] shows the age wise distribution of all the neoplastic lesions.
| Age | Number of patients |
| 0-10 years | 4 |
| 11-20 years | 2 |
| 21-30 years | 11 |
| 31-40 years | 6 |
| 41-50 years | 9 |
| 51-60 years | 13 |
| 61-70 years | 14 |
| >70 years | 3 |
Table 2 shows the various histological types of tumors in our study including rare types.
| Most common benign lesions | Renal Oncocytoma |
| Most common malignant lesions | Wilms’ tumor Clear Cell Renal Cell Carcinoma Liposarcoma Lymphnode metastasis |
| Rare benign lesions | Adrenal Myelolipoma Multiple Paragangliomas Benign Fibrous Histiocytoma Fibrolipomatous Hamartoma |
| Rare malignant lesions | De-differentiated Liposarcoma Clear Cell Sarcoma of Kidney Carcinosarcoma of Kidney Malignant GIST Adult onset Wilms’ tumor |
We attempted to classify retroperitoneal tumors encountered in pediatric age group and Table 3 illustrates the histological diagnosis of these tumors and the age group in which they were seen.
| S.No | Age/sex | Diagnosis |
| 1. | 15y/F | Metastatic Dysgerminoma |
| 2. | 8y/F | Malignant Mixed Germ Cell Tumor (Embryonal carcinoma + Yolk sac tumor) |
| 3. | 2y/F | Classic triphasic Wilms’ tumor |
| 4. | 3y/M | Clear Cell Sarcoma of Kidney |
| 5. | 15 days/M | Fibrolipomatous Hamartoma |
Discussion
Malignant tumors of retroperitoneum are four times more frequent than benign tumors. In our study also malignant tumors outnumbered benign tumors with a ratio of 2:1. This ratio is in sharp contrast to neoplastic disease occurring elsewhere in the body, where benign disease predominates.[4]
In the current study tumors occurred predominantly in the 5th and 6th decades with a male, female ratio of 1.13:1. Tumor size in most cases was >15cm with an average size of 12cm. Liposarcoma constituted the common histological type followed by Renal Cell Carcinoma and Lymph node metastases. Routine histological examination with clinical correlation aided in diagnosis of most of the cases, some requiring special stains and IHC. The age and sex incidence in our study was concordant with other studies in literature and are depicted in [Table 4].
| Parameters | Stoeckle et al, 20018 | Van Dalen et al, 20015 | Lewis et al, 1998 6 | Gronchi et al, 20047 | Present study, 2018 |
| Number of patients | 165 | 142 | 500 | 165 | 62 |
| Male : Female ratio | 1.0:1.2 | 1.01:1.22 | 1.34:1.0 | 1.2:1.0 | 1.13:1 |
| Age (years) | |||||
| Median | 54 | 60 | 58 | 53 | 60 |
| Range | 16-82 | 18-88 | 16-88 | 15-82 | 15 days-74 |
We encountered many rare tumors in the retroperitoneum, both benign and malignant. Adrenal Myelolipomas are extremely rare tumors, benign in nature and composed of a variable mixture of mature adipose tissue and hematopoietic elements.[9] We diagnosed a case of Adrenal Myelolipoma in a 60-year-old male who presented with pain in upper abdomen and had the characteristic histological picture.
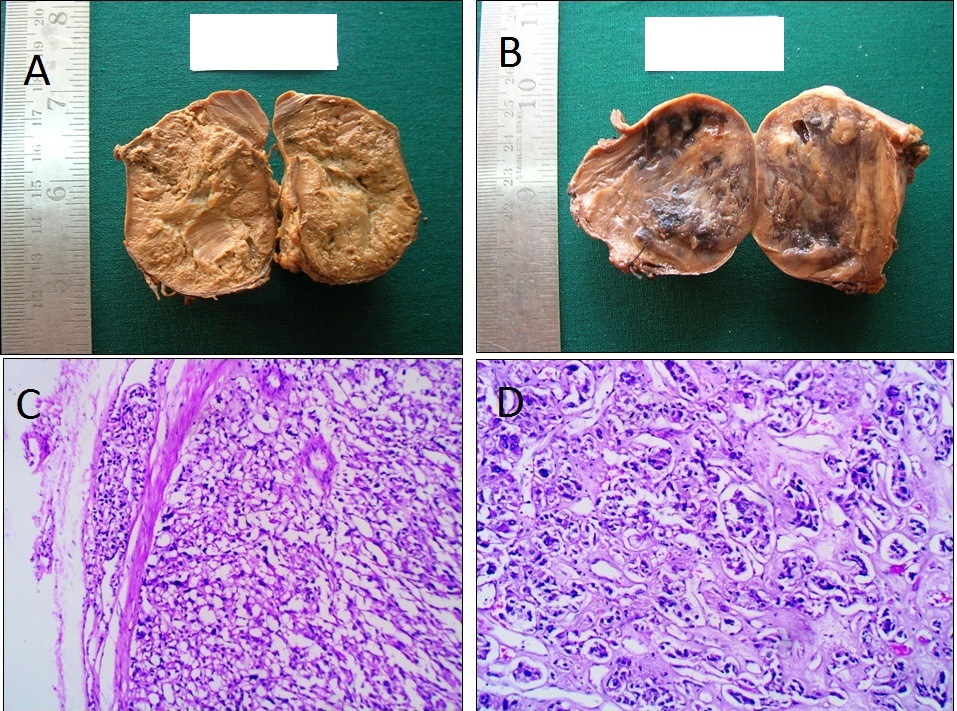
We reported a rare case of multiple Paragangliomas in a 40-year-old woman who presented with a history of throbbing headache and fever. On examination she was found to be hypertensive with ultrasound of abdomen showing two tumors, one in the left suprarenal region and the other at the region of the aortic bifurcation. Both the specimens received were 5x4.5x4cm with cut section showing encapsulation, grey tan and grey yellow areas ([Figure 1]A,B). Microscopically the tumors were similar with neoplastic cells arranged in the characteristic Zell-ballen patterns and also showed lymphovascular emboli in the pericapsular area ([Figure 1]C,D). IHC by Chromogranin and Synaptophysin for tumor cells, S- 100 for the sustentacular cells. Santosh R et al reported multiple Paragangliomas in a 14-year-old girl with similar locations as in our study.[10]
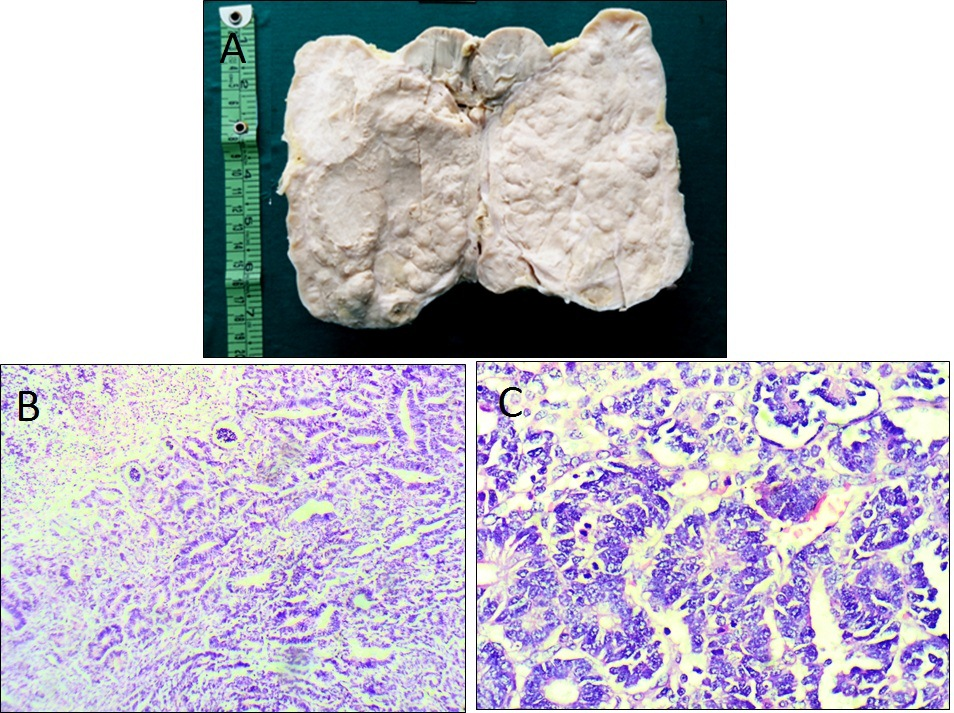
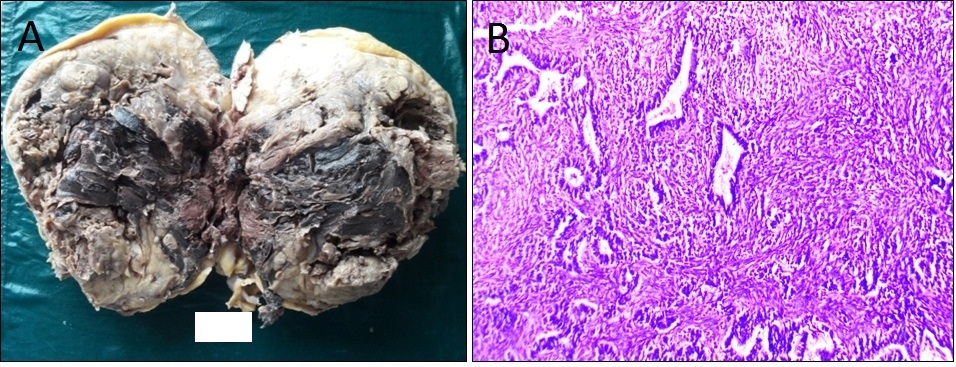
Only 3% of Wilms’ tumors are reported in adults and most are diagnosed un-expectedly following nephrectomy for presumed Renal Cell Carcinoma.[11] A 53-year-old male presented with left flank pain and fever for 2 months. On examination a huge tender mass was palpable in the left side of abdomen with CT scan showing a large heterogeneous mass in the left kidney. Nephrectomy was performed and the specimen received showed a tumor almost replacing the entire kidney. The tumor was solid, partially lobulated with a variegated appearance ([Figure 2]A). Microscopy revealed Wilms’ tumor with biphasic histology and epithelial predominance. Majority of the tumor showed primitive tubule and glomeruli formation admixed with a minimal mesenchymal component ([Figure 2]B,C). Varma et al described a Triphasic Wilms’ tumor in a 48-year-old male with similar clinical presentation.[11]
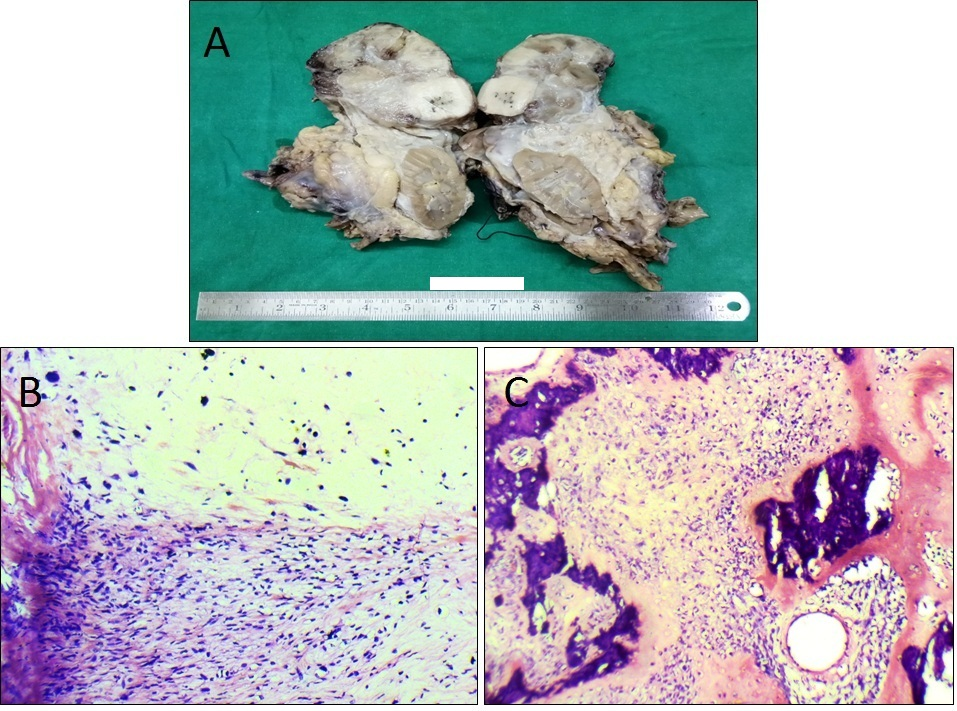
De-differentiation in a Liposarcoma can be an Undifferentiated Pleomorphic Sarcoma or resemble a carcinoma, melanoma, meningioma or a nerve sheath tumor. Chondrosarcomatous and Osteosarcomatous elements may also be seen.[12] A 58-year-old male patient presented with a mass in retroperitoneal region with loss of weight. An abdominal contrast-enhanced computerized tomography (CECT) revealed a large encapsulated mass. Surgery was done and specimen received was of size 18x15x12cm with cut section showing yellow-tan areas admixed with firm tan-gray areas ([Figure 3]A). Microscopically the tumor displayed areas of Well Differentiated Liposarcoma and non-lipogenic components of Mesenchymal Chondrosarcoma and Osteosarcoma. The interphase between the two zones was typically abrupt.
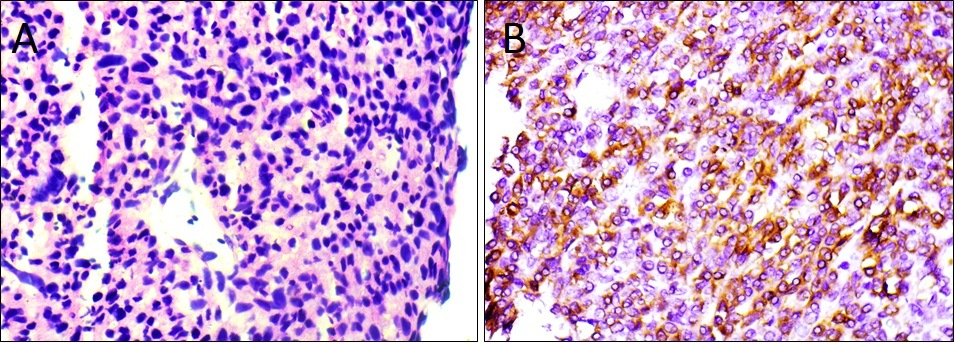
Gastrointestinal stromal tumors (GISTs) are the most common mesenchymal neoplasms of the gastrointestinal tract. Rarely they occur outside the gastrointestinal tract (omentum, mesentery and retroperitoneum) and are called Extra-gastrointestinal stromal tumors (EGISTs).[13] We reported a case of EGIST in retroperitoneum of a 64-year-old male patient. He presented with back pain since 4 months and CT scan showed a retroperitoneal solid mass in left paravertebral region. Microscopically the tumor was cellular and composed of sheets of round to ovoid cells with scant eosinophilic cytoplasm & dense nuclear chromatin ([Figure 4]A). The mitotic count was <5/50 High power fields (HPF) (Low mitotic activity). IHC showed positivity for CD117 ([Figure 4]B).
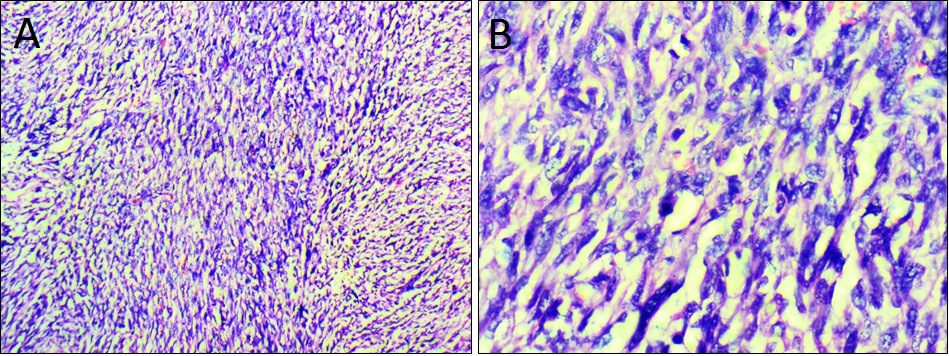
We also encountered a case of Malignant GIST in a 50-year-old male who presented with complaints of progressive pain abdomen for 4 months. CECT scan revealed a lobulated solid mass lesion in the retroperitoneum with necrotic areas. Ultrasound guided needle core biopsy showed a malignant spindle cell neoplasm with high cellularity, fascicular growth pattern and large areas of necrosis ([Figure 5]A). Tumor showed high grade cellular features with mitotic activity of >10 per 50 HPF ([Figure 5]B). The tumor demonstrated classical CD117 positive features on IHC.
We reported a rare case of Carcinosarcoma of the kidney in a 56-year-old male patient who presented with right flank pain and hematuria. Surgery was done after radiological confirmation. We received a nephrectomy specimen with a tumor almost occupying the entire kidney ([Figure 6]A). Microscopically the tumor was composed of malignant glandular & sarcomatoid components with a Ki-67 index of 40% ([Figure 6]B). Xiu-Peng Zhang et al reported a similar case of Carcinosarcoma occurring in the renal pelvis in a 56-year-old male patient. In their case the tumor also showed chondroid and osteoid components which were not observed in our case.[14]
For all our cases of soft tissue sarcomas we used the FNCLCC grading system developed by The French Federation of Cancer Centers Sarcoma Group which is based on the three histological parameters including tumor differentiation, mitotic rate and tumor necrosis.
Conclusion
To conclude, in our study malignant tumours were higher in distribution than benign tumours in both pediatric and adult age groups. The commonest epithelial tumour being Renal Cell Carcinoma and mesenchymal tumour being Well Differentiated Liposarcoma. Immunohistochemistry using an appropriate panel of antibodies was done to arrive at a definitive diagnosis. Rare tumours of epithelial & mesenchymal origin were encountered both in adult & childhood age group.
Acknowledgements
Nil
Funding
Nil
Competing interests:
Nil
References
- C Brennan, D Kajal, K Khalili, S Ghai. Solid malignant retroperitoneal masses-a pictorial review. Insights Imaging 2013. [Google Scholar]
- Siva Ranjith, M S Sulfekar, Subhash. Retroperitoneal Sarcoma -A Clinico-Pathological Study. IOSR-JDMS 2017. [Google Scholar]
- D C Strauss, A J Hayes, J M Thomas. Retroperitoneal tumours: Review of management. Ann R Coll Surg Engl 2011. [Google Scholar]
- J F Van Roggen, P C Hogendoorn. Soft tissue tumours of the retroperitoneum. Sarcoma 2000. [Google Scholar]
- T Dalen, H J Hoekstra, A N Van Geel. Dutch Soft Tissue Sarcoma Group. Locoregional recurrence of retroperitoneal soft tissue sarcoma: second chance of cure for selected patients. Eur Surg Oncol 2001. [Google Scholar]
- J J Lewis, D Leung, J M Woodruff, M F Brennan. Retroperitoneal soft-tissue sarcoma: analysis of 500 patients treated and followed at a single institution. Ann Surg 1998. [Google Scholar]
- A Gronchi, P G Casali, M Fiore. Retroperitoneal soft tissue sarcomas: patterns of recurrence in 167 patients treated at a single institution. Cancer 2004. [Google Scholar]
- E Stoeckle, J M Coindre, S Bonvalot. Prognostic factors in retroperitoneal sarcoma: a multivariate analysis of a series of 165 patients of the French Cancer Center Federation Sarcoma Group. Cancer 2001. [Google Scholar]
- J Nabi, D Rafiq, F Authoy, G N Sofi. Incidental Detection of Adrenal Myelolipoma colon-A Case Report and Review of literature. Case Rep Urol 2013. [Google Scholar]
- R Santosh, K Subas, J Kini, N Bhat, S Rao. Multiple Rretroperitoneal Paragangliomas. Indian J Surge 2013. [Google Scholar]
- A V Varma, K Malukani, P Rihal, S S Nandedkar. Adult Wilms tumor : A case report with review of literature. J Can Res Ther 2015. [Google Scholar]
- R John Goldblum, Andrew L Folpe, Sharon W Weiss, M Franz Enzinger. In Enzinger and Weisss Soft tissue tumors. 2014. [Google Scholar]
- C Claudioc, V Vincenzov, D A Filippoda, C Manuelac, S Bruno. Primary Extra-gastrointestinal Stromal Tumor of Retroperitoneum. Clinical Medical Insights. Oncol 2012. [Google Scholar]
- Xiu-Peng Zhang, Qin Zheng, Chen Wang, Liang Wang, Yang Liu, Qing-Chang Li. Carcinosarcoma of the renal pelvis with prominent heterologous elements mimicking teratoma: A case report and literature review. Int J Clin Exp Med 2017. [Google Scholar]
How to Cite This Article
Vancouver
Vaishnavi R, Naik BS, Premalatha P, Ramya C, Renuka IV. Rare tumors of retroperitoneum-A diagnostic challenge [Internet]. Indian J Pathol Oncol. 2025 [cited 2025 Sep 08];6(4):671-676. Available from: https://doi.org/10.18231/j.ijpo.2019.127
APA
Vaishnavi, R., Naik, B. S., Premalatha, P., Ramya, C., Renuka, I. V. (2025). Rare tumors of retroperitoneum-A diagnostic challenge. Indian J Pathol Oncol, 6(4), 671-676. https://doi.org/10.18231/j.ijpo.2019.127
MLA
Vaishnavi, Ranuva, Naik, Bandavat Sankar, Premalatha, P, Ramya, Ch, Renuka, I V. "Rare tumors of retroperitoneum-A diagnostic challenge." Indian J Pathol Oncol, vol. 6, no. 4, 2025, pp. 671-676. https://doi.org/10.18231/j.ijpo.2019.127
Chicago
Vaishnavi, R., Naik, B. S., Premalatha, P., Ramya, C., Renuka, I. V.. "Rare tumors of retroperitoneum-A diagnostic challenge." Indian J Pathol Oncol 6, no. 4 (2025): 671-676. https://doi.org/10.18231/j.ijpo.2019.127
