- Visibility 93 Views
- Downloads 11 Downloads
- DOI 10.18231/j.ijpo.2019.114
-
CrossMark
- Citation
Ki67 labeling in CNS tumours
- Author Details:
-
Manjiri Karandikar
-
Narayanan Subramanian Mani
-
Uttara Mani *
Introduction
The Ki67 antigen was originally identified by Scholzer and Gerdes in the early 1980s as a proliferation associated nuclear antigen, which coincides with the transit of cells through mitosis.[1] Some studies have shown a correlation of its expression with p 53 in oral and breast cancers and potential as a reliable prognostic marker in cancers of breast, lung, CNS, prostate and cervix.[2] An increasing number of studies have suggested immunohistochemical staining for Ki67 to be important for grading in many tumor types. Ki67 labeling index (LI) has also been used as a diagnostic tool for high grade colonic and pancreatic cancers. Some workers feel that it is however best used as a prognostic marker due to its advantages over conventional markers. Studies have shown correlation between its expression and prognostic markers like lymphatic invasion, metastasis and tumor size.
Scoring systems using antibodies rely on the percentage of stained tumor cells. One study has described scoring in at least 8 fields in a tumor at x20 magnification. Other studies have shown Ki67 LI cutoff levels between 10 and 14% to define poor prognosis. The St Gallen consensus in 2009 used Ki67 LI for addition of chemotherapy in the treatment of hormone receptor positive breast cancers. Tumors may also be classified as low (</ =15%), intermediate (16-30%) and highly proliferative (>30%) using the Ki67 LI.[3]
The current classification scheme of CNS tumours is not optimal because of variation in parameters such as tumor heterogeneity, sampling errors and tumors with common histology. Measurement of proliferative activity is important in determining the grade and likelihood of recurrence of astrocytomas and mitotic indices are used often as a marker of proliferative potential. But this is subject to interobserver variability and not consistent to differentiate low and high grade tumors. Current studies suggest Ki67 and AGNOR evaluation as the simplest and most reliable of these techniques.[4] Immunohistochemical evaluation of Ki67 LI has been suggested as a vital diagnostic and prognostic tool in the assessment of biological behavior of astrocytomas and is important in determining grade and likelihood of recurrence.
Johannessen and Torp reviewed the literature on Ki67 LI in astrocytomas and brought out that most studies differentiated well between grade II and grade III astrocytomas and glioblastomas. It may be useful in cases where histology reveals a low grade astrocytoma whereas other parameters indicate a more malignant neoplasm.[5] Shivaprasad et al demonstrated an increase of Ki67 LI with increasing grade of the tumor in 30 astrocytomas they studied. A naplastic astrocytomas (grade III) and glioblastomas showed a mean Ki67 LI of 6.58% and 17.81% respectively. Some glioblastomas also showed low indices and hence they suggest that Ki67 alone may not be sufficient for this purpose. They found a statistically significant difference between grade II and grade III astrocytomas but no difference between grade III tumors and glioblastomas.[6] Thotakura et al demonstrated significant differences in Ki67 LI between all grades of astrocytomas except grade I and grade II in their study of 105 cases.[7] Other studies by Montine et al, Wakimoto et al and Rathi et al have demonstrated a significant relation between tumor grade and Ki-67 LI.[8]
Various authors suggest that the wide differences in Ki67 LI may be partially explained by variable sensitivities of detection methods like peroxidase antiperoxidase, avidine, dilutions of antibodies and antigen retrieval methods and inter observer counting variability and that laboratories should set up their own range of values for different grades.[7] In view of the above, this study aimed to determine the utility of Ki67 LI in the overall assessment of CNS neoplasms.
Materials and Methods
This was a retrospective and prospective study of all CNS tumors received at Dept of Pathology of this medical college hospital between Aug 2013 and July 2018. Patient case records were obtained and details noted. Paraffin blocks of retrospective cases were retrieved from the department archives. Fresh paraffin sections were cut. Fresh tissues of prospective cases received at the Department of Pathology were processed as per standard histopathological techniques and stained by the H&E technique. All these cases were classified histopathologically as per the WHO classification of CNS Tumors of 2016 and graded as per WHO criteria. 47 cases were studied in this series. Cases which were n on-representative and showed predominantly necrotic tissue were excluded.
Immunohistochemistry
3 µm sections were prepared on Poly-L-lysine precoated slides. A ntigen retrieval was performed in EnVision FLEX Target retrieval solution (Low pH(50x) (Code K8005) of DAKO) by microwaving at 97ºC twice for 10 min. Slides were then exposed to EnVision Blocking reagent H2 O2 for 30 min, covered with primary antibody (ready to use-monoclonal mouse antibody Clone: MIB-1 Isotype: IgG1, kappa) for 2 hours. After washing with PBS buffer secondary antibody was applied for 1 hour. Sections were washed and exposed to 1500 µl substrate + 48 µl Diaminobenzidine (DAB) for 3 min till brown colour developed in the sections, to a maximum of 5 min. Sections were counterstained with Harris’ Haematoxylin stain, cleared and mounted. Ki67 LI was determined by counting the number of stained nuclei per 500 neoplastic cells in tissue sections. The histopathological features and Ki67 LI were correlated with clinical and radiological data and with the WHO grade.
Results
95 cases of CNS tumours were received in this department during the period of study of which 47 cases were suitable for immunohistochemistry. These 47 cases comprised 22 WHO Grade I neoplasms (46.8 %) and 25 neoplasms of WHO Grade II or higher (53.2 %). 39 cases (8 2.9 %) occurred in the brain and 8 (17%) occurred in the spinal cord. 21 cases (44.7%) occurred in m ales and females comprised 26 (55.3%). 5 cases occurred in the 0-14 age group, 1 in an adolescent (15-19years) and 41 cases in adults. The youngest case occurred at 4½ months of age and the oldest at 78 years.
5 meningiomas, 2 ependymomas and 1 plasmacytic lymphoma occurred in the spinal cord. 3 cases (2 meningiomas and 1 tanycytic ependymoma) occurred purely at the cervical cord producing various degrees of cord compression. The dorsal cord was affected in 4 cases with 3 meningiomas (psammomatous, clear cell and cystic meningioma) and a lymphoplasmacytic lymphoma. The only lumbosacral case was a myxopapillary ependymoma.
[Table 1] shows the distribution of 39 neoplasms occurring in the brain. 9 of 23 cases in the cerebral hemispheres showed involvement of adjacent lobes either contiguously or as multiple foci. Parietal and temporal lobes were most commonly affected with 13 and 10 cases respectively. These comprised 6 Grade I, 8 Grade II, 1 Grade III and 7 Grade IV neoplasms. All grade IV neoplasms were Glioblastomas of which 4 occurred in the temporal lobes. Cerebellopontine (CP) angle neoplasms were most commonly meningiomas and schwannomas. Pituitary lesions were most common in the sellar region. Infratentorial neoplasms comprised hemangioblastomas and ependymomas most commonly.
22 of the neoplasms were graded as WHO Grade I, 13 as Grade II, 3 as Grade III and 9 as Grade IV. 13 meningiomas comprised the most common neoplasm in grade I neoplasms followed by hemangioblastomas, pituitary adenomas and schwannomas. The Grade II neoplasms comprised most commonly diffuse astrocytomas (5 cases) followed by ependymomas, atypical meningiomas, oligodendrogliomas and pleomorphic xanthoastrocytomas (PXA). The grade III neoplasms compris ed a case each of anaplastic PXA, anaplastic papillary meningioma and choroid plexus carcinoma each. 9 cases were grade IV neoplasms comprising mostly glioblastomas.
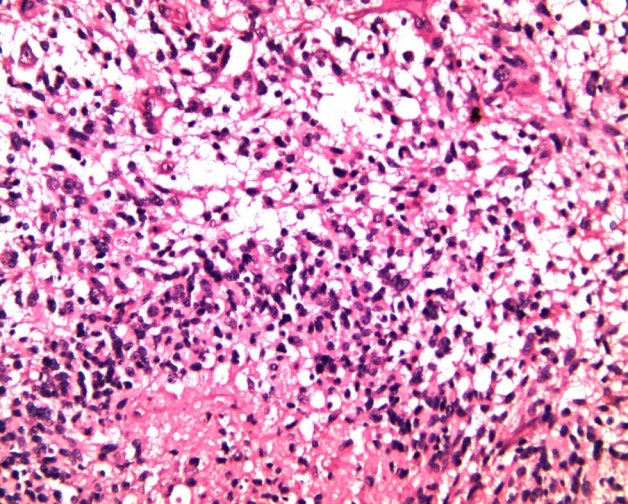
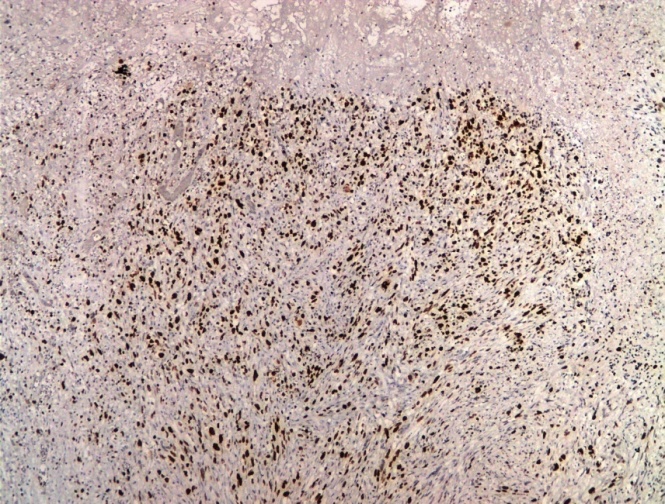
A strocytic and oligodendroglial tumours comprised 16 cases (34%) of the neoplasms studied. 5 of these were diffuse astrocytomas, NOS, 7 Glioblastomas, NOS, 2 Oligodendrogliomas, NOS and 2 were circumscribed astrocytomas (PXAs). All 5 diffuse astrocytomas,NOS were Gde II neoplasms with Ki67 LI varying from 0.72 to 13.9% with a mean of 4.36%. 7 glioblastomas, NOS showed varying histological patterns with small tumor cells, spindle cell sarcomatous change and tumor giant cells. Ki67 LI varied from 5.96 to 22.4 % with a mean of 12.26% ([Figure 1],[Figure 2]). The 2 oligodendrogliomas showed Ki67 LI of 0.59% and 9.26% with a mean of 4.92%. Both the PXAs occurred in children and showed large ballooned astrocytes and giant cells along with foamy cells. Ki67 LI was 0.63% in one case. The other case had an LI of 21.66% and was reclassified as an anaplastic PXA WHO Grade III.
4 ependymomas comprised 1 conventional, 2 tanycytic and 1 myxopapillary ependymoma. Ki67 LI varied from not detectable to 3.96% with a mean of 1.33. The spinal case was a clear cell variant but showed a low Ki67 LI.
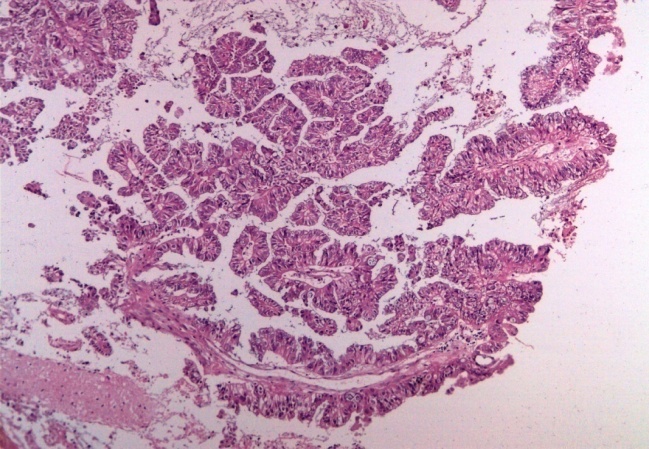
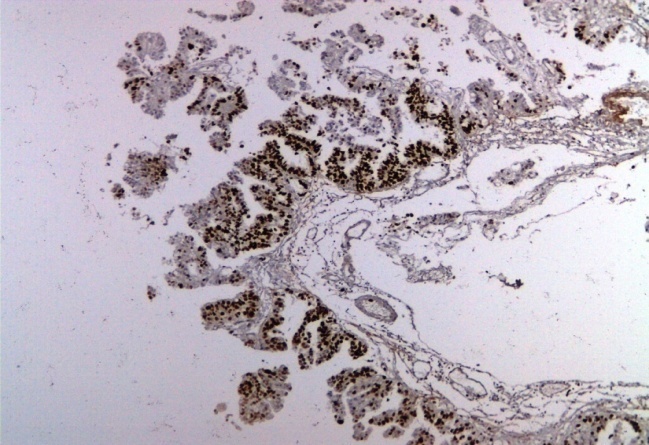
13 of 16 meningiomas were grade I and the Ki67 LI varied from nil to 5.48% with a mean of 2.22%. 2 were grade II atypical meningiomas with 9.82% and 1.89% Ki67 LIs and 1 grade III papillary meningioma had a Ki67 LI of 30% ([Figure 3],[Figure 4]). Necrosis was seen in grade II and grade III meningiomas. 2 schwannomas studied showed Ki67 LI of 3% and 7.63%. The choroid plexus carcinoma occurred in a 45 year old and showed highly atypical tall columnar cells in papillary pattern with hyperchromatic nuclei and necrosis. The Ki67 LI was 60% ([Figure 5],[Figure 6]).
Both the cerebellar hemangioblastomas occurred in elderly adults and showed typical histopathology. Ki67 LI were 1.32 % and 4.38%. Of the 2 Non-Hodgkins’ lymphomas o ne case occurred in a 78 year old female and was suggestive of a lymphoplasmacytic lymphoma, which was confirmed with CD 138. Ki67 LI was very high at 64.1%. The second case occurred in a 60 year old female as a corpus callosal growth. This case was CD20 positive and diagnosed as a diffuse large B cell lymphoma of the CNS with a very high Ki67 LI of 91%. 2 pituitary adenomas in this study showed cells in sheets, acinar and trabecular patterns with psammoma bodies and perivascular pseudorosettes. Ki67 LI was 0.35% and 0.89% in these cases. The Ki67 LIs of various neoplasms are summarized at [Table 2] along with WHO grade.
| Location | Number | Diagnosis & Number |
| Cerebral Hemispheres | 23 | Meningioma- 7 Oligodendroglioma-2 Diffuse astrocytoma-5 Glioblastoma-7 PXA-2 |
| Cerebello Pontine Angle | 6 | Schwannoma-2 Choroid plexus carcinoma-1 Ganglioglioma-1 Meningioma-2 |
| Infratentorial | 6 | Ependymoma-2 Meningioma-1 Hemangioblastoma-2 Glioneuronal tumour-1 |
| Sellar | 3 | Pituitary adenoma-2 Meningioma-1 |
| Midline | 1 | Diffuse large BCL |
| S No | WHO Grade | Histological diagnosis | Number | Ki67 index range(%) | Mean Ki67 index(%) |
| 1 | I | Meningiomas | 13 | 0-5.48 | 2.22 |
| Hemangioblastoma | 2 | 1.32-4.38 | 2.85 | ||
| Pituitary Adenoma | 2 | 0.35-0.89 | 0.62 | ||
| Schwannoma | 2 | 3-7.63 | 5.3 | ||
| Ganglioglioma | 1 | 0.79 | 0.79 | ||
| Glioneuronal tumour | 1 | 0 | 0 | ||
| Myxopapillary ependymoma | 1 | 3.96 | 3.96 | ||
| Total | 22 | 2.32 | |||
| II | Diffuse Astrocytoma, NOS | 5 | 0.72-13.9 | 4.36 | |
| Ependymoma | 3 | 0-1.06 | 0.49 | ||
| PXA | 1 | 0.63 | 0.63 | ||
| Atypical meningioma | 2 | 1.89-9.82 | 5.85 | ||
| Oligodendroglioma | 2 | 0.59-9.26 | 4.92 | ||
| Total | 13 | 3.5 | |||
| III | Anaplastic PXA | 1 | 21.66 | 21.66 | |
| Anaplastic meningioma | 1 | 30 | 30 | ||
| Choroid plexus carcinoma | 1 | 60 | 60 | ||
| Total | 3 | 37.22 | |||
| IV | Glioblastoma | 7 | 5.96-22.4 | 12.26 | |
| Non Hodgkins lymphoma | 2 | 64-91 | 77.5 | ||
| Total | 9 | 26.75 |
| WHO Grade | Yan et al (n/%) | This study (n/%) |
| I | 23/ 6.4% | 0/% |
| II | 91/25.3% | 8/50% |
| III | 95/26.4% | 1/6.25% |
| IV | 151/41.9% | 7/43.7% |
| Total | 360 | 16 |
| Authors | Diffuse astrocytoma Gr II (n/ Mean Ki67 LI) | Anaplastic astrocytoma (n/ Mean Ki67 LI) | Glioblastoma (n/ Mean Ki67 LI) |
| Karamitopoulou et al | 24/ 2.03 | 26/ 12.8 | 9/14.6 |
| Khalid et al | 24/1.78 | 20/13.5 | 33/15.7 |
| Salimen et al | 8/6.26 | 13/16.6 | |
| Wakimoto et al | 19/3.8 | 25/18.4 | 28/31.6 |
| Di et al | 29/1.2 | 25/9 | 24/12 |
| Hsu et al | 16/0.88 | 31/8.7 | 33/9.12 |
| Enestrom et al | 6/ 7.6 | 9/13.3 | 7/24.3 |
| Hilton et al | 96/1.15 | - | - |
| McKeever et al | 50/<2 in 22 cases & >2in 28 cases | - | - |
| This study | 5/4.36 | - | 7/12.3 |


Discussion
This retrospective and prospective observational study of Ki67 LI by immunohistochemistry in 47 CNS neoplasms showed a greater proportion of neoplasms Grade II and higher. This is in contrast to figures from the United States where two thirds of CNS tumours were diagnosed as non malignant. However in this study cystic lesions such as epidermoid cysts have been excluded which may account for this difference.
Malignant gliomas and meningiomas were the most common groups of CNS tumours comprising 34% each. This contrasted with the study by Ostrom et al.[9] in which meningiomas were the most common at 35.6%. Astrocytic and oligodendroglial tumours as per the WHO classification 2016 were the most common group comprising 16 cases[10] of which the most common were glioblastoma, NOS and diffuse astrocytoma, NOS Grade II ([Table 3]).
The greatest discrepancy was seen in Grade II and III tumours when comparing this study with that of Yan et al.[11] This study showed a higher proportion of cases in Grade II(50 vs 25.3%) and lower in Grade III (6.25 vs 26.4%) as compared to the study by Yan et al.
5 cases of diffuse astrocytomas in this study showed Ki67 LI range from 0.72 to 13.9% with a mean of 4.36%. Mean LIs in Grade II diffuse astrocytomas have varied from 1.15 to 7.6% in various studies ([Table 3]) and our finding was comparable. Thotakura et al in their study of 105 astrocytomas showed an LI of 7.05+/-4.16 in grade II astrocytomas and 38.7+/-7.2 in grade IV Glioblastomas. They demonstrated significant differences in Ki67 LI between all grades of astrocytomas except grade I and grade II.[7]
7 glioblastomas in this study showed varying mitoses and additional features such as the presence of multinucleate giant cells, small cells and spindle cell sarcomatous component as described in literature.[12] The Ki67 LIs varied from 5.96 to 22.4% with a mean of 12.3% which was comparable with various studies where the mean proliferation indices varied from 9.12 to 31.6 ([Table 4]).[8]
Oligodendrogliomas (ODG) are composed of oligodendrocyte like tumor cells along with microcalcification and a delicate branching capillary network. The 2 typical oligodendrogliomas in this study showed moderate to high cellularity and microcalcifications. Mean Ki67 LI was 4.92% +/- 4.37%. The case with higher index did not show nuclear atypia or mitotic activity but showed gemistocytic change and giant cells. Kros et al have reported gliofibrillary oligodendrocytes to show a higher Ki67 LI. [13]
The pleomorphic xanthoastrocytoma (PXA) showed typical histological features with circumscription, large pleomorphic multinucleated cells with spindle and lipidized cells, dense pericellular reticulin network and numerous eosinophilic granular bodies. 1 case had a high index of 21.66% and was reclassified as an anaplastic PXA. Gianini et al have shown that the Ki67 LI is generally less than 1% in PXAs.[14]
3 histological variants of ependymomas (papillary, clear cell and tanycytic) are described and were encountered in this study.[15],[16] The myxopapillary ependymoma shows the presence of elongated fibrillary processes arranged around fibrovascular cores with a Ki67 LI.[17] The LI in this case was 3.96%. The clear cell ependymoma shows an oligodendrocyte like appearance with perinuclear halos due to cytoplasmic clearing.[18] The Ki67 LI in this case was 1.06%. Both tanycytic variants showed tumor cells in fascicles and elongated cells with spindled nuclei[19] (Fig 14). Ki67 done in both these cases were low at 0% and 0.4%.
Meningiomas are slow growing tumors that are graded from Grades I to III.[10] 16 meningiomas in this study comprised 13 WHO grade I, 2 WHO grade II and 1 WHO grade III. Cellular proliferation increases proportionate to grade. Perry et al have shown that a Ki67 LI of >4% in meningiomas increased the risk of recurrence and >20% increased the death rates.[20] 6 of 16 meningiomas in this study showed LIs of >4% and a greater likelihood of recurrence and aggressive behavior. Ho et al have shown MIB1 ranges of 0.7-2.2% for benign, 2.1-9.3% for a typical and 11-16.3% for anaplastic meningiomas.[21] This study has shown a mean of 2.22% for benign, 5.85% for atypical and 30% for the single case of anaplastic meningioma which is comparable. However the numbers were too few to suggest cutoff LIs.
1 case of choroid plexus carcinoma occurred in a middle aged male. Ki67 LIs have been reported from 4.1-60% for choroid plexus carcinoma as per Vajtai et al and Carlotti et al[22],[23] and the LI done in this case was 60%.
Gangliogliomas are WHO grade Iglioneuronal neoplasms composed of dysplastic ganglion cells along with neoplastic glial cells with Ki67 LI of 1.1-2.7% as reported by Luyken et al and other studies.[24] Our case had a lower LI of 0.79%. The glioneuronal tumor was composed of astroglial cells and round cells possibly neurocytes which occurred in a 4 month male who presented with a seizure disorder and a hypothalamic mass. The Ki67 LI is reported as <3%[25] and our case showed undetectable Ki67 positivity. Both the schwannomas in this study were composed entirely of well differentiated Schwann cells with Antoni A and Antoni B areas. Pekmezci et al have shown a cutoff of 20% for malignancy.[26] Mean Ki 67 LI was 5.3%+/- 2.3%.
Haemangioblastomas are defined as WHO grade I tumors characterized by neoplastic stromal cells and abundant small vessels. Both the hemangioblastomas in this study occurred in elderly patients in the cerebellum and presenting as cystic lesions with mural nodules. There is a dearth of reports of Ki67 LI in haemangioblastoma. Our cases showed a mean LI of 2.85%+/-1.5. The pituitary adenomas in this study showed a mean LI of 0.62%+/- 0.27. They are now classified as per pituitary adenohypophyseal cell lineage into acidophilic, corticotroph and gonadotroph lineages.[27] Mean Ki67 LI was 0.62%+/-0.27.
The 2 haematopoietic neoplasms in this study were a Diffuse large B cell lymphoma of the CNS and a lymphoplasmacytic Non Hodgkins Lymphoma. The Ki67 LI of DLBCL of the CNS is described as varying from 70-90%[28] and was 91% in our case. The lymphoplasmacytic Non Hodgkins lymphoma was confirmed with CD 138 and also showed a high Ki67 LI of 64.1%.
Conclusion
To conclude, this study of Ki67 LI in 47 CNS neoplasms was found to correlate well with WHO CNS tumour grade and helped to identify histologically defined lower grade tumours with potential for recurrence and progression. However differences in technique and interpretation make it difficult to establish a definitive cutoff point for accurate translation from one laboratory to another. Ki67 immunohistochemistry is recommended for all CNS neoplasms with suspicious histopathological features. This study will add to the literature on the subject of proliferative markers in the Indian context.
Source of funding
None.
Conflict of interest
None
References
- T Scholzen, J Gerdes. The Ki-67 protein: from the known and the unknown. J Cell Physiol 2000. [Google Scholar]
- T Nakano, T Ohno, H Ishikawa. Current advancement in radiation therapy for uterine cervical cancer. J Radiat Res 2010. [Google Scholar]
- Y Hayashi, H Takei, M Kurosumi. Ki67 immunohistochemical staining :The present situation of diagnostic criteria. Nihon Rinsho 2012. [Google Scholar]
- Q H Alfredo, N Sanai, J S Smith, W Mcdermott. Techniques to assess the proliferative potential of brain tumors. J Neuro Oncol 2005. [Google Scholar]
- A L Johannessen, S H Torp. The clinical value of Ki-67/MIB-1 labelling index in human astrocytomas. Pathol Oncol Res 2006. [Google Scholar]
- N V Shivaprasad, S Satish, S Ravishankar, M G Vimalambike. Ki-67 immunostaining in astrocytomas: association with histopathological grade-a South Indian study. J Neurosci Rural Pract 2016. [Google Scholar]
- M Thotakura, N Tirumalasetti, R Krishna. Role of Ki-67 labelling index as adjunct to the histopathological diagnosis and grading of astrocytomas. J Can Res Ther 2014. [Google Scholar]
- K R Rathi, B D Radotra, V K Khosla. Proliferative index in astrocytic tumors. Indian J Pathol Microbiol 2007. [Google Scholar]
- - Qt, H Gettlemen, P Liao, C Rouse. CBTRUS statistical report: primary brain and CNS tumours diagnosed in the United States in. Neuro Oncol 2007. [Google Scholar]
- D N Louis, H Ogaki, O D Wiestler, W K Cavenee, D W Ellison. . WHO Classification of tumours of the Central Nervous System 2016. [Google Scholar]
- H Yan, D W Parsons, Jen G Mclendon, R Etal. IDH1 and IDH2 mutations in gliomas. N Engl J Med 2009. [Google Scholar]
- . Burger PC, Kleuhues P Cytologic composition of the untreated glioblastoma with implication for evaluation of needle biopsies. Cancer 1989. [Google Scholar]
- J M Kros, K Degrieve, A Van Tilburg. Hop W et al NF2 status of meningioma in association with tumour localization and histology. J Pathol 2001. [Google Scholar]
- C Giannini, B W Scheithauer, P C Burger, D J Bratt. Pleomorphic xanthoastrocytoma: what do we really know about it?. Cancer 1999. [Google Scholar]
- D E Godfrain, J M Kaczmarska, M Kochak, J Dalton. Distinct disease risk griups in paeditric supratentorial and posterior fossa ependymomas. Acta Neuropathol 2012. [Google Scholar]
- K W Pajtler, H Witt, M Sill, D T Jones. Molecular classification of ependymal tumours across all CNS compartments, histopathological grades and age groups. Cancer Cell 2015. [Google Scholar]
- . Flament-Durant J, Brion JP Tanycytes: morphology and function: a review. Int Rev Cytol 1985. [Google Scholar]
- T A Dolecek, J M Propp, N E Stroup. Kruchkoc CBTRUS statistical report: primary brain and CNS tumours diagnosed in the United States in 2005-2009. Neuro Oncol 2012. [Google Scholar]
- A Olar, K M Wani, E P Sulman, A Mansouri. Mitotic index in an independent predictor of recurrence free survival in meningioma. Brain Pathol 2015. [Google Scholar]
- A Perry, S L Stafford, B W Scheithaeur. Suman VJ et al Meningioma grading, an analysis of histological parameters. Am J Surg Pathol 1997. [Google Scholar]
- D M Ho, C Y Hsu, L T Ting, H Chiang. Histopathology and MIB-1 labeling index predicting recurrence in meningiomas. Cancer 2002. [Google Scholar]
- I Vajtai, Z Varga, A Aguzzi. MIB-1 immunoreactivity reveals different labeling in low grade and in malignant epithelial neoplasms of the choroid plexus . Histopathol 1996. [Google Scholar]
- C G Carlotti, B Salhia, F Weitzman, N Greenberg. Evaluation of proliferation index and cell cycle protein expression of choroid plexus tumours in children. Acta Neuropathol 2002. [Google Scholar]
- C Luyken, I Blumcke, R Fimmers, H Urbach. Supratentorial gangliogliomas: histopathological grading and tumour recurrence in 184 patients with a median follow up of 8 years. Cancer 2004. [Google Scholar]
- M Preusser, W Dietrich, T Czech. Prayer D et al Rosette forming glioneuronal tumour of the IVth ventricle. Acta Neuropathol 2003. [Google Scholar]
- M Pekmezci, D E Reuss, A C Hirbe, S Dahiya. Morphologic and immunohistochemical features of malignant peripheral nerve sheath tumours and cellular schwannomas. Mod Pathol 2015. [Google Scholar]
- R Y Osamura, Mbs Lopez, A Grossman, A Matsuno, R V Lloyd. Pituitary adenoma. . (EDS) WHO classification of tumours of endocrine organs 2017. [Google Scholar]
- U Schlegel. Primary CNS lymphoma. Ther Adv Neurol Disord 2009. [Google Scholar]
