- Visibility 177 Views
- Downloads 39 Downloads
- DOI 10.18231/j.ijpo.2019.101
-
CrossMark
- Citation
Role of basic haematological investigations in the evaluation of pancytopenia
- Author Details:
-
Poornakala S
-
Kavitha Ravi *
Introduction
Pancytopenia is not a disease, but a triad of Anaemia, Leucopoenia and Thrombocytopenia. It is caused by various disease processes which affect the bone marrow primarily or secondarily.[1] It can be due to single or different co -existing pathology. The various underlying mechanisms of Pancytopenia include decreased hematopoietic cell production due to destruction of marrow tissue, replacement of bone marrow by abnormal or malignant tissue, ineffective haematopoiesis with cell death in bone marrow, formation of defective cells which are rapidly removed from circulation, sequestration or destruction of cells by the action of antibodies, and trapping of normal cells in hypertrophied reticuloendothelial system.[2]
As the management and prognosis depends on underlying pathology and the severity of Pancytopenia, identification of correct aetiology is crucial and helps in appropriate treatment.[3],[4] Detailed clinical evaluation, routine complete blood count with indices and a peripheral blood film are required as a part of initial evaluation, as a battery of laboratory tests are essential for accurate diagnosis. Hence the current study intends to study the etiological profile of Pancytopenia and to identify the complete blood count (CBC), peripheral smear (PS)findings which are helpful in narrowing the differential diagnosis and in planning the additional investigations to arrive a specific diagnosis.
Study setting and design
Descriptive study conducted in a tertiary care centre in Kerala. As it was a retrospective study, patient consent was not needed and there were no ethical issues.
Materials and Methods
Inclusion criteria includes Hemoglobin < 10 g / dl, Total leukocyte count < 4000 / mm3 and Platelet count < 1, 00,000 / mm3. Exclusion criteria were cases with inadequate bone marrow material and cases where a definite diagnosis could not be offered in bone marrow. 132 Cases of Bone marrow aspirates which satisfied the inclusion criteria, received during a period of 18 months from January 2011 to June 2012 were studied.
The etiological profile was studied. The clinical features studied include Age, sex distribution, and presence of Pallor, Hepatomegaly and Splenomegaly. Hematological parameters studied include Hemoglobin, Total Leukocyte count and Platelet count. Median value of these parameters in each category was compared. Peripheral smear findings were evaluated in detail. RBC morphology findings included the presence of Anisopoikilocytosis, Polychromasia and nucleated RBCs. WBC morphology included presence of Hyper segmented neutrophils, Relative Lymphocytosis and Presence of Blasts.
Results
One hundred and thirty two pancytopenia cases were studied. The Etiology profile observed in this study is given in [Figure 1]. The most common cause of Pancytopenia in the present study is Sub leukemic leukemia (23.5%) followed by Hypersplenism (17.4%) and Meg aloblastic Anemia(14.3%). Other common aetiologies include Hypoplastic Anemia(10.6%), Myelodysplastic Syndrome(MDS) (9.1%), Myelofibrosis (7.6%) and Autoimmune cytopenias(AIHA) (6.1%). Less frequent etiologies observed include Multiple Myeloma, Hemophagocytic syndrome (HPS), Tuberculosis, Malaria, Iron deficiency Anemia and Chronic myeloid leukemia on Imatinib.
Age distribution, sex distribution, frequency of Hepatomegaly, Splenomegaly in different etiologies are shown in [Table 2]. The youngest patient was 12 years old, a case of Acute leukemia and the oldest patient was 88yrs old, a case of Hypersplenism. The common age group varied with different etiology. Overall, Males and Females were almost equal in distribution with male to female ratio 1.03:1 However Megaloblastic anemia showed male preponderance and Hypoplastic anemia Autoimmune cytopenias showed female preponderance. Pallor was observed in almost all the cases. Hepatomegaly was observed in 19% cases with frequent occurrence in MDS and acute leukemia. Splenomegaly was seen in 28% cases with frequent occurrence in Hypersplenism followed by autoimmune cytopenias.
The median values of Hemoglobin, Total Leukocyte count, and Platelet count in various etiologies are summarized in the [Table 3]. Lowest median Hemoglobin was observed in Megaloblastic Anemia whereas Leucopenia and Thrombocytopenia were severe in Hypoplastic Anemia.
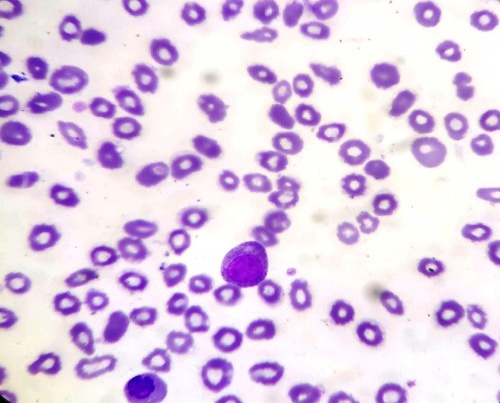
Peripheral smear findings in various etiologies are summarized in the . Among the RBC findings Anisopoikilocytosis, Polychromasia and circulating nucleated RBCs were predominant in Megaloblastic Anemia. Among the WBC findings, Hypersegmented neutrophils were observed predominantly in Megaloblastic anemia and in a single case of MDS. Relative Lymphocytosis was predominant in Hypoplastic anemia and MDS whereas Immature WBCs, in particular blasts were seen commonly in acute leukemia.
Discussion
The proportion of cases in different aetiologies of Pancytopenia varies with difference in methodology, diagnostic criteria, and period of observation, geographic area, age, nutritional status, genetic differences, and exposure to infections, myelotoxic agents and other factors.[4]
Megaloblastic anaemia and Hypoplastic anaemia are the commonest causes of Pancytopenia in various studies conducted all over the world. In the current study Sub leukemic leukaemia was the most common aetiology accounting to (23.5%) followed by Hypersplenism (17.4%) and Megaloblastic Anemia (14.3%). Though Sub leukemic leukaemia as the most common cause of Pancytopenia is uncommon, similar observations were seen in studies conducted by Jalaeikhoo et al (35.4%) and Keisu et al.[5],[6] Pancytopenia can be seen in approximately 30% cases of acute leukaemia at the time of initial presentation.[2] The percentage of cases in the current study parallels the observations of Jhaet al (21.6%), Makheja et al (27.4%) and Mallick et al (30.5%).[7],[8],[9] Hepato megaly was common in sub leukemic leukaemia than other aetiology which could be due to tumour infiltration. Immature WBCs in particular, Blasts were observed in 87% cases in Peripheral smear in spite of Pancytopenia which parallels the observation of Devi et al and Khunger et al who observed immature WBCs in 71% cases and 100% cases respectively.[10],[11] Thus in the setting of Pancytopenia with organomegaly and presence of immature WBC in PS, sub leukemic leukaemia should be considered with high index suspicion and Bone marrow study along with Immunophenotyping should be sought for confirmation and typing.
Incidence of hypersplenism as a cause of Pancytopenia in different studies varies from 3–68%.[4] Hypersplenismcan be caused by various reasons like portal hypertension, infections and may haematological disorders. Dameshk proposed four criteria for diagnosis of hypersplenism, which includes splenomegaly, one or several types of cytopenias, bone marrow normal or in hyperplastic state and disappearance of cytopenias after splenectomy.[12] In the present study, Splenomegaly was observed in 69.5% cases and the degree of anaemia was mild when com pared to other aetiology. PS was characterised by absence of immature RBCs, WBCs and relative lymphocytosis was seen only in 4% cases indicating the neutrophilic predominance. If hypersplenism is detected clinically and in PS, only bone marrow aspirate is sufficient for diagnosis.[13] It helps to rule out the neoplastic causes of splenomegaly and splenectomy can be planned which is curative for cytopenias.[14]
Megaloblastic anaemia is the commonest cause of Pancytopenia in majority of Indian studies. It is caused by deficiency of Vitamin B12 or folate or both which are essential for DNA synthesis and their deficiency causes disordered cell proliferation.[13] In the present study the degree of anaemia was severe in megaloblastic anaemia compared to other aetiology and hepatosplenomegaly was observed in 21% cases which are due to extra medullary haematopoiesis. PS showed anisopoikilicytosis in 89% cases similar to observations of Pereira et al and Javalgi who observed APS in all cases.[15],[16] Also the proportion of cases with presence of immature RBCs is higher when compared to other aetiology indicating stress erythropoiesis to severe anaemia. Among WBC findings Hyper segmented neutrophils was observed in 63% cases whereas Khodke et al and Tilak et al observed in 91% cases and 84.9% cases respectively.[2],[3] Tilak et al suggested that bone marrow examination could be deferred in Pancytopenia cases presenting with hepatosplenomegaly (HSM) and hyper-segmented neutrophils in PS. These patients can be put on haematinics with close follow up.[3] Elevated lactate dehydrogenase (LDH) is consistently observed in megaloblastic anaemia. It is the result of accelerated turnover of bone marrow cells implying the release of this enzyme from dividing/decaying cells. Para R observed elevated LDH in 74 % cases, which was also, observes by Eivazi-Ziaei et al.[1],[17]
A plastic anaemia accounted for 10.6% cases and showed lowest median value of leucopoenia and thrombocytopenia similar to the observations of Yadav et al.[18] Peripheral smear showed relative lymphocytosis in 86% cases, similar to the observations of Tilak et al (50%) Khunger et al (85.7%).[3],[11] This finding supports the fact that aplastic anaemia is immune mediated with active destruction of blood forming cells by lymphocytes. The abnormal immune response is triggered by variety of factors like viral infections, chemicals, drugs etc. Hence, in Pancytopenia cases with severe cytopenias along with macrocytic anaemia, reticulocytopenia and relative lymphocytosis in PS, Aplastic anaemia should be suspected strongly. It helps to plan bone marrow biopsy, as aspirations are frequently dry tap.
Incidence of MDS in the present study is 9.1 %, which parallels the observation of Pereira et al.[15] Khunger et al observed MDS in 2% cases where as Devi et al observed in 18% cases who also noted presence of immature WBCs in all cases.[10],[11] PS in majority cases of MDS showed Anisopoikilocytosis with relative lymphocytosis and presence of immature WBCs. Recent studies suggest that autoimmunity plays role in MDS pathophysiology and younger age group MDS patients responded better to immunosuppression. [19],[20]
In Primary myelofibrosis, in the fibrotic stage of disease, patients have Pancytopenia along with massive splenomegaly. Blood smear is leucoerythroblastic with marked anisopoikilocytosis including teardrop shaped RBCs. In the present study, 30% cases showed hepatosplenomegaly and LEBP in peripheral smear. All the cases showed fibrosis in reticulin staining ranging from grade 2 to grade 4. Hence, in Pancytopenia cases with organomegaly and LEBP in PS, Bone marrow biopsy along with reticulin staining should be planned, as aspirates are frequently dry tap.
Autoimmune diseases can present with Pancytopenia, which can have multiple etiological factors.[14] The underlying pathology includes autoimmune destruction, bone marrow suppression, hypersplenism and drugs. In cases with autoimmune haemolytic anaemia, the peripheral smear demonstrates spherocytes, polychromasia, normoblast and RBC agglutinates which is a valuable clue in suspecting autoimmune aetiology.[21]
| Diagnosis | Common Age group | Sex predominance | Hepatomegaly | Splenomegaly |
| Acute leukaemia | 3rd, 5th and 6th | M | 10(32%) | 9(29%) |
| Hypersplenism | 4th | F | 3(13%) | 16(69.5%) |
| Megaloblastic Anaemia | 3rd ,5th | M | 4(21%) | 3(16%) |
| Hypoplastic Anaemia | 2nd | F | 1(7%) | 0 |
| MDS | 7th | M | 4(33%) | 2(16%) |
| Myelofibrosis | 6th, 7th | M | 3(30%) | 3(30%) |
| Autoimmune cytopenias | 2nd | F | 0 | 4(50%) |
| Diagnosis | Total cases | Haemoglobin | Total count | Platelet count |
| Acute leukaemia | 31 | 6.6 | 2500 | 38000 |
| Hypersplenism | 23 | 8.5 | 2700 | 63000 |
| Megaloblastic Anaemia | 19 | 4.9 | 2600 | 27000 |
| Hypoplastic Anaemia | 14 | 7.3 | 1400 | 27000 |
| MDS | 12 | 5.7 | 3300 | 41000 |
| Myelofibrosis | 10 | 5.9 | 1900 | 37000 |
| Autoimmune cytopenias | 8 | 6.6 | 2600 | 100000 |
| Diagnosis | Total cases | APS | Poly | Normoblast |
| Acute leukaemia | 31 | 10(32%) | 8(26%) | 10(32%) |
| Hypersplenism | 23 | 13(56%) | 1(4%) | 0 |
| Megaloblastic Anaemia | 19 | 17(89%) | 11(58%) | 10(52%) |
| Hypoplastic Anaemia | 14 | 8(57%) | 2(14%) | 0 |
| MDS | 12 | 10(83%) | 7(58%) | 3(25%) |
| Myelofibrosis | 10 | 3(30%) | 7(70%) | 3(30%) |
| Autoimmune cytopenias | 8 | 5(62%) | 5(62%) | 2(25%) |
| Diagnosis | Total cases | Hyper segmented neutrophils | Relative lymphocytosis | Blasts |
| Acute leukaemia | 31 | 0 | 11(35%) | 27(87%) |
| Hypersplenism | 23 | 0 | 1(4%) | 0 |
| Megaloblastic Anaemia | 19 | 12(63%) | 5(26%) | 0 |
| Hypoplastic Anaemia | 14 | 0 | 12(86%) | |
| MDS | 12 | 1(8%) | 5(42%) | 3(25%) |
| Myelofibrosis | 10 | 0 | 3(30%) | 3(30%) |
| Autoimmune cytopenias | 8 | 0 | 2(25%) | 0 |

Multiple myeloma as a cause of Pancytopenia was observed in 9% cases in study conducted by Subrahmanyam et al.[13] Sridevi et al observed an average of 63% of plasma cells in bone marrow of the multiple myeloma patients presented with Pancytopenia.[22] PS showed normocytic normochromic anaemia and the rouleaux form at ion were evident in 90% cases. Pancytopenia in multiple myeloma patients carries therapeutic significance because these patients will require a mandatory addition of dexamethasone in order to avoid stem cell damage by alkylating agents.[23]
Hemophagocytic syndrome as a cause of PCP is seen in 2.3% cases. Tilak et al and Pereira et al have reported cases of HLH in their study.[3],[5] The underlying aetiology can be primary or secondary and cytopenias in one or more lineage is one of the criteria for diagnosis. Malaria especially, Plasmodium falciparum causes Pancytopenia. However, case reports are available emphasising P. vivax infection in Pancytopenia, which is due to associated hemophagocytosis.[24],[25] Pancytopenia associated with Tuberculosis is reported in various studies.[26],[27] This proves the prevalence of TB in India and the necessary to be aware of its manifestation as Pancytopenia.



Conclusion
The diagnosis of Megaloblastic anaemia is possible by blood counts, RBC indices, Peripheral smear findings and Biochemical tests. If vitamin B12 and folate estimation for confirmation is not possible due to cost factor, bone marrow examination can be deferred and these patients can be put on haematinics with close follow up.
In cases with immature WBCs in particular Blast in PS, Bone marrow examination should be done at the earliest as Sub leukemic leukaemia, MDS and Myelofibrosis are the common underlying causes, which need early intervention.
Severe cytopenias in CBC along with macrocytic anaemia and relative lymphocytosis in peripheral smear prompts /warrants aplastic anaemia and hence bone marrow biopsy should be planned along with aspiration
Rare causes like HIV infection, Tuberculosis and Multiple myeloma should be kept in mind in evaluating the Pancytopenia patients.
Physical examination, CBC and peripheral blood picture play an important role in planning further investigations in Pancytopenia patients. As many causes of Pancytopenia are treatable and curable, accurate diagnosis and timely intervention decides the prognosis.
Acknowledgements
Nil.
Conflicts of interest
Nil.
References
- R Para, S Para. Pancytopenia-a study of 58 cases. J Evol Med Dent Sci 2013. [Google Scholar]
- K Khodke, S Marwah, G Buxi, R B Yadav, N K Chaturvedi. Bone marrow examination in cases of Pancytopenia. J Academy Clin Med 2001. [Google Scholar]
- V Tilak, R Jain. Pancytopenia--a clinico-hematologic analysis of 77 cases. Indian J Pathol 1999. [Google Scholar]
- A Jain, M Naniwadekar. An etiological reappraisal of Pancytopenia-largest series reported to date from a single tertiary care teaching hospital. BMC Blood Disord 2013. [Google Scholar]
- H Jalaeikhoo, S M Kashfi, P Azimzadeh, A Narimani, K G Moghadam. Acute Myeloid Leukemia as the Main Cause of Pancytopenia in Iranian Population. Iran J Pathol 2017. [Google Scholar]
- M Keisu, A Ost. Diagnoses in patients with severe Pancytopenia suspected of having aplastic anemia. Eur J Haematol 1990. [Google Scholar]
- A Sayami, G Adhikari, R C Panta, A D Jha, R .. Bone marrow examination in cases of Pancytopenia. J Nepal Med Assoc 2008. [Google Scholar]
- K D Makheja, B K Maheshwari, S Arain, S Kumar, S Kumari. The common causes leading to Pancytopenia in patients presenting to tertiary care hospital. Pak J Med Sci 2013. [Google Scholar]
- M Mallik, R Bhartiya, S Mallick, R Singh, M Kumar, R V Singh. Pancytopenia-a study of clinico-haematological profile in adults with its bone-marrow co-relation in a tertiary hospital of Bihar. Int J Contemp Med Res 2016. [Google Scholar]
- P M Devi, R S Laishram, P S Sharma, A M Singh, M K Singh. Clinico-hematological profile of Pancytopenia in Manipur, India. Kuwait Med J 2008. [Google Scholar]
- J M Khunger, S Arulselvi, U Sharma, S Ranga, V H Talib. Pancytopenia--a clinico haematological study of 200 cases. Indian J Pathol Microbiol 2002. [Google Scholar]
- Y Lv. Causes of peripheral blood cytopenias in patients with liver cirrhosis portal hypertension and clinical significances. J Endocrine Metab Dis 2014. [Google Scholar]
- Y Subrahmanyam, M Padma. Pancytopenia a three years evaluation. Int J Sci Res 2015. [Google Scholar]
- E P Weinzierl, D A Arber. The differential diagnosis and bone marrow evaluation of new-onset Pancytopenia. Am J Clin Pathol 2013. [Google Scholar]
- A D Pereira, A Dias. Hematological Analysis of Pancytopenia: A Prospective Study. Int J Sci Stud 2016. [Google Scholar]
- A P Javalgi, V D Dombale. Clinico-hematological analysis of Pancytopenia: A bone marrow study. Natl J Lab Med 2013. [Google Scholar]
- J Eivazi-Ziaei, S Dastgiri, Z Sanaat. Estimation of the diagnostic value of myeloperoxidase index and lactate dehydrogenase in megaloblastic anaemia. J Clin Diagn Res 2007. [Google Scholar]
- S Yadav, R Kushwaha, K Aggrawal, A K Tripathi, U S Singh, A Kumar. A clinico-hematological study in cases of pancytopenia: correlation of automated cell counter parameters in various etiologies. J Evol Med Dent Sci 2013. [Google Scholar]
- A J Barrett, E Sloand. Autoimmune mechanisms in the pathophysiology of myelodysplastic syndromes and their clinical relevance. . [Google Scholar]
- M E Chamuleau, T M Westers, L Van Dreunen, J Groenland, A Zevenbergen, C M Eeltink. Immune mediated autologous cytotoxicity against hematopoietic precursor cells in patients with myelodysplastic syndrome. Haematol 2009. [Google Scholar]
- C H Packman. The clinical pictures of autoimmune hemolyticanemia. Transfus Med Hemother 2015. [Google Scholar]
- H B Sridevi, S Rai, P K Suresh, M S Somesh, J Minal. Pancytopenia in multiple myeloma-an enigma: our experience from tertiary care hospital. J Clin Diagn Res 2015. [Google Scholar]
- D E Reece. Management of multiple myeloma: the changing landscape. Blood reviews 2007. [Google Scholar]
- S Pothapregada, B Kamalakannan. Hemophagocytic syndrome in Plasmodium vivax malaria. J Vector Borne Dis 2014. [Google Scholar]
- . Acute plasmodium vivax malaria presenting with pancytopenia secondary to hemophagocytic syndrome: case report and literature review. J Fam Community Med 2009. [Google Scholar]
- V Bachkaniwala, J Thorat, A Gupta, R Parikh, D Dave, P Kashyap, P Melmane. Unusual case of tuberculosis. Int J Res Med Sci 2017. [Google Scholar]
- R Avasthi, D Mohanty, S C Chaudhary, K Mishra. Disseminated tuberculosis: interesting hematological observations. J Assoc Physicians India 2010. [Google Scholar]
How to Cite This Article
Vancouver
S P, Ravi K. Role of basic haematological investigations in the evaluation of pancytopenia [Internet]. Indian J Pathol Oncol. 2019 [cited 2025 Sep 11];6(4):520-525. Available from: https://doi.org/10.18231/j.ijpo.2019.101
APA
S, P., Ravi, K. (2019). Role of basic haematological investigations in the evaluation of pancytopenia. Indian J Pathol Oncol, 6(4), 520-525. https://doi.org/10.18231/j.ijpo.2019.101
MLA
S, Poornakala, Ravi, Kavitha. "Role of basic haematological investigations in the evaluation of pancytopenia." Indian J Pathol Oncol, vol. 6, no. 4, 2019, pp. 520-525. https://doi.org/10.18231/j.ijpo.2019.101
Chicago
S, P., Ravi, K.. "Role of basic haematological investigations in the evaluation of pancytopenia." Indian J Pathol Oncol 6, no. 4 (2019): 520-525. https://doi.org/10.18231/j.ijpo.2019.101
