- Visibility 301 Views
- Downloads 39 Downloads
- Permissions
- DOI 10.18231/j.ijpo.2021.071
-
CrossMark
- Citation
Histopathological spectrum of oral cavity lesions – A tertiary care experience
Abstract
Background: Oral cancer is one of a major health problem in some parts of the world especially in the developing countries. Oral cancer is the sixth most common cancer in the world whereas in India it is one of the most prevalent cancer. Oral cavity lesions are usually asymptomatic. Accurate diagnosis of the lesion is the first step for the proper management of patients and histopathology is considered as the gold standard.
Aims: The objective is to study the different patterns of oral cavity lesions seen in a tertiary care hospital of Jammu
Study Design: One year retrospective study.
Setting: Post graduate department of pathology.
Materials and Methods: It was a retrospective study carried out in a tertiary care centre for a period of one year from March 2020 to Feb 2021. 148 cases of oral cavity lesions were included in this study. The parameters that were included in the study were sociodemographic data, site of the lesion, clinical features and histological diagnosis. Data collected was analysed.
Results: 148 cases of oral lesions were identified during the period of study. The age of patients varied from 5 to 78years and Male to Female ratio was 2.2:1. Buccal mucosa (30%) was the most common site involved which was followed by tonsil (19%). Out of 148 cases 70 cases were malignant, 10 cases pre malignant and 21 cases were benign. Squamous cell carcinoma (33.7%) was the most common lesion present in our study.
Conclusions: Oral cavity lesions have a vast spectrum of diseases which range from tumour like lesions to benign and malignant tumours. Our study concluded that squamous cell carcinoma was the most common malignant lesion of oral cavity. Histological typing of the lesion is important for confirmation of malignancy and it is essential for the proper management of the patient.
Introduction
The oral cavity is the entry point for the upper aero-digestive tract, which starts at the level of lips and ends at the anterior surface of the faucial arch. It is lined by keratinizing or non – keratinizing stratified squamous epithelium with a few minor salivary glands. The oral cavity is at continuous exposure to both inhaled and consumed carcinogens and therefore it is one of the most common site for the origin of malignant neoplasms.
The most common carcinogenic agents associated with the oral cavity lesions are tobacco, alcohol, and betel nuts. The primary tumours of the oral cavity can arise from the surface epithelium (stratified squamous epithelium), minor salivary glands or submucosal soft tissues. The most common tumor of oral cavity is Squamous cell carcinoma, and the rest are the tumors of minor salivary gland and other rare tumours.
The cancer of the oral cavity is more common in men. In the western part of the world, the most common sites for origin of primary squamous cell carcinoma of oral cavity are tongue and the floor of the mouth. However, in the developing countries where the chewing of tobacco and betel nuts is common, the retromolar trigone and buccal mucosa are the most frequently encountered primary sites for oral cancers.[1]
In India oral cancer is a major health problem and it ranks third among all the cancers of the country.[2] Many studies have reported that excessive intake of alcohol and tobacco are a major risk factor for developing oral and pharyngeal tumours.[3] There is a high prevalence of chewing tobacco mixtures in India, thus contributing to increased incidence of oral cancers.[4]
The lesions of the oral cavity are very common. These can be benign or malignant. The most common benign lesions of the oral cavity are lymphoid hyperplasia, retention cyst, inflammation, haemangioma, fibroma etc. And among malignant lesions Squamous cell carcinoma is the most common. Oral cancer ranks 8th worldwide and it is 3rd most common cancer in India. 12.6 per 100,000 population is the age standardized incidence rate of oral cancer.[5]
Even though lesions of oral cavity can be easily reached for direct examination these malignancies still remain undetected for a long time. Accurate diagnosis of the pre-malignant and malignant oral lesion marks the first step for the proper management of the patient. Histopathology is still the gold standard.[6] The present retrospective study was carried out to study the different patterns of oral cavity lesions.
Materials and Methods
This retrospective study was carried out in the Department of Pathology of Government Medical College and Hospital, Jammu during the period of one year from March 2020 to February 2021. The study included all the patients admitted in the ENT and/or Surgery ward of the hospital presenting with oral pathology. Findings of clinical history and physical examination were noted from patient records. The parameters included in the study were age, gender, site and histopathological diagnosis of the lesion. All the biopsy specimens of oral cavity lesions were included in the study. Any repeat biopsy for residual lesion after therapy was excluded from the study. The data collected was analysed.
Results
A total of 148 cases of oral cavity lesions were studied. The age varied from 5 years to 78 years. A five-year-old male child with chronic tonsillitis was the youngest patient and the 78 years old male with Squamous cell carcinoma of buccal mucosa was the oldest one. Majority of patients were in the age range of 40-60 years. Among 148 cases 70(47.2%) cases were malignant, 10 cases (6.75%) were pre-malignant, 21 (14.18%) cases were benign and 47(31.7%) cases were non –neoplastic ([Table 1]).
Out of total 148 cases, 102 (68.9%) were males and 46 (31%) were females with a Male: Female ratio of 2.21:1. The most common clinical presentations were ulcero-proliferative growth, ulcers, nodular growth and proliferative growth.
Buccal mucosa was the commonest site involved (30%) followed by tonsil (19%), tongue (17%), floor of mouth (13%) and palate (11%). Malignant lesions were restricted to buccal mucosa, tongue, tonsil and minor salivary glands in floor of mouth. All the tongue lesions turned out to be malignant ([Figure 1]).
Majority of the non-neoplastic lesions were chronic inflammatory lesions (14.18%) followed by chronic tonsillitis (8.1%). Among the benign neoplasms benign keratosis was the commonest. Premalignant lesions encountered were 4 cases of keratosis with mild dysplasia, 3 cases of keratosis with moderate dysplasia, 2 cases of carcinoma in situ and 1 case of submucosal fibrosis. In our study squamous cell carcinoma was the most common malignant lesion of oral cavity ([Table 2]).
|
Age (years) |
Non neoplastic lesions |
Benign |
Pre-malignant |
Malignant |
Total |
|
0-9 |
1 |
|
|
|
1 |
|
10-19 |
9 |
5 |
|
1 |
15 |
|
20-29 |
7 |
3 |
- |
3 |
13 |
|
30-39 |
7 |
5 |
1 |
12 |
25 |
|
40-49 |
9 |
5 |
3 |
18 |
35 |
|
50-59 |
5 |
3 |
2 |
15 |
25 |
|
60-69 |
9 |
- |
1 |
14 |
24 |
|
70-79 |
- |
- |
2 |
3 |
5 |
|
80-89 |
- |
- |
1 |
4 |
5 |
|
Total |
47 |
21 |
10 |
70 |
148 |

|
Type of lesion |
Number (n) |
Percentage (%) |
|
Non - Neoplastic |
||
|
Chronic inflammatory lesion |
21 |
14.18 |
|
Chronic tonsillitis |
12 |
8.1 |
|
Epulis |
3 |
2.0 |
|
Lichen Planus |
4 |
2.7 |
|
Epidermal cyst |
4 |
2.7 |
|
Retention cyst |
3 |
2.0 |
|
Benign |
||
|
Pyogenic granuloma |
3 |
2.0 |
|
Hemangioma |
5 |
3.3 |
|
Pleomorphic adenoma |
3 |
2.0 |
|
Fibroma |
2 |
1.3 |
|
Benign keratosis |
8 |
5.4 |
|
Pre – malignant |
||
|
Submucosal fibrosis |
1 |
0.6 |
|
Keratosis with mild dysplasia |
4 |
2.7 |
|
Keratosis with moderate dysplasia |
3 |
2.0 |
|
Carcinoma in situ |
2 |
1.3 |
|
Malignant |
||
|
Squamous cell carcinoma |
50 |
33.7 |
|
Basal cell carcinoma |
8 |
5.4 |
|
Adenoid cystic carcinoma |
2 |
1.3 |
|
Verrucous carcinoma |
5 |
3.3 |
|
Basosquamous carcinoma |
5 |
3.3 |
|
Total |
148 |
100 |



Discussion
This retrospective study was done to study the distribution of various lesions of oral cavity. The age range of the study subjects was 5 to 78 years. This is in concordance to many studies conducted in the different parts of the world. In our study, the oral mucosal lesions were more frequently seen in males than in females, which is similar to the study done by Pudasaini S et al.[7]
In our study the malignant neoplastic lesions (47.26%) accounted for maximum number of cases, an observation similar to that reported by Modi et al.[8] It was seen that neoplastic lesions are also more common in males than in females with M: F ratio of 2.21:1 which is similar to the findings of Pudasaini S and Brar R who observed a ratio of 2:1.[7] This can be attributed to more unhygienic oral habits especially in males of this region. Oral mucosal lesions were more prevalent in the age group of 30 to 69 years, probably due to the long standing oral habits of use of tobacco during this age. In the present study it was observed that the incidence of oral cancer increases with age which was similar to the observation of Modi et al., and Malaovalla et al.[8], [9]
The most common site involved in our study was Buccal mucosa (30%), which was followed by tonsil (19%), tongue (17%). This is in concordance to the study done by Modi et al.[8] and Mehta et al.[10] who reported similar findings. In another study done by Mehrotra et al.[11] it was found that Buccal mucosa was the most frequently involved site followed by tongue for benign and premalignant lesions of oral cavity.
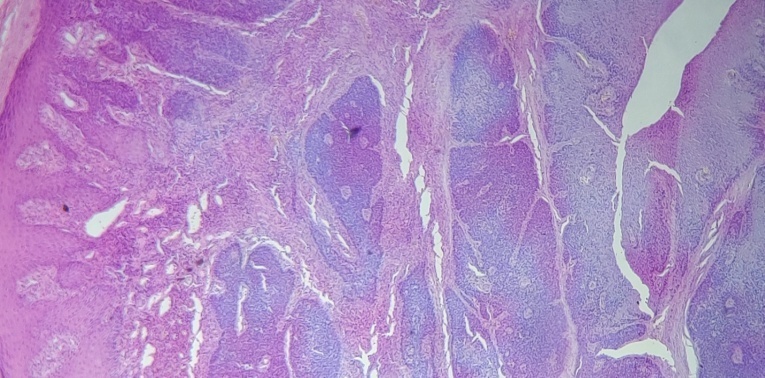
Most of the lesions of squamous cell origin have a varying degree of histologic progression which begins from mild dysplasia – moderate dysplasia – carcinoma in situ - invasive carcinoma. The histologic grade of the lesion denotes the aggressive nature of the tumour. Squamous cell carcinoma may range from well differentiated to poorly differentiated as well as undifferentiated and sarcomatoid This is defined by the extent of tumour differentiation, nuclear pleomorphism, cytological atypia, and morphologic resemblance to the benign squamous mucosa. Undifferentiated or sarcomatoid tumors are more aggressive in nature. Squamous cell carcinoma (33.7%) was the most common malignant lesion ([Figure 4]) encountered in our study. The most common site involved was buccal mucosa followed by tonsil. Similar results were also seen in the studies done by Misra et al.[12] and Hassawi et al.[13]
Early diagnosis of pre-cancerous and cancerous lesions of oral cavity can be done much easily as it is an easily accessible site for examination. However, the most important step to reduce the incidence of oral cancer is to prevent the use of tobacco or its products. Many new research techniques have been used for increasing the sensitivity and specificity of detection rate of oral lesions especially malignancy but all of these have their own limitations. These diagnostic tests include – Toluidine blue staining, oral brush cytology, tissue reflectance, narrow emission tissue fluorescence, tumour markers and molecular diagnostic techniques.[14], [15]
Conclusion
The lesions of oral cavity include a wide array of lesions which range from tumour like lesions to benign and malignant tumours. Our study concluded that squamous cell carcinoma was the most common malignant lesion of oral cavity. Histopathological examination of oral biopsies is an important tool for the early diagnosis and management of the lesions.
Source of Funding
None.
Conflict of Interest
The authors declare that there is no conflict of interest.
References
- Shah J, Patel S, Singh B. Oral cavity. Head and neck surgery and oncology. 2007. [Google Scholar]
- Elango J, Gangadharan P, Sumithra S. Trends of head and neck cancers in urban and rural India. Asian Pac J Cancer Prev. 2006;7(1):108-12. [Google Scholar]
- Madani A, Jahromi A, Dikshit M. Risk assessment of tobacco types and oral cancer. Am J Pharmacol Toxicol. 2010;5(1):9-13. [Google Scholar]
- Gupta P, Ray C. Smokeless tobacco and health in India and South Asia. Respirology. 2003;8(4):419-31. [Google Scholar] [Crossref]
- Petersen P. Strengthening the prevention of oral cancer: the WHO perspective. Community Dent Oral Epidemiol. 2005;33(6):397-9. [Google Scholar]
- Poh C, Samsung N, Berean K, Williams P, Rosin M, Zhang L. Biopsy and histopathologic diagnosis of oral premalignant and malignant lesions. J Can Dent Assoc. 2008;74(3):283-8. [Google Scholar]
- Pudasaini S, Barar R. Oral cavity lesions: A study of 21 cases. J Pathol Nepal. 2011. [Google Scholar]
- Laishram R, Modi D, Sharma L, Debnath K. Pattern of oral cavity lesions in a tertiary care hospital in Manipur, India. J Med Soc. 2013;27(3):199-202. [Google Scholar] [Crossref]
- Malaowalla A, Silverman S, Mani N, Bilimoria K, Smith L. Oral cancer in 57,518 industrial workers of Gujarat, India.A prevalence and followup study. Cancer. 1976;37(4):1882-6. [Google Scholar] [Crossref]
- Mehta N, Dave K, Gonsai R. Histopathological study of oral cavity lesions: a study on 100 cases. Int J Res Rev. 2013;5:110-6. [Google Scholar]
- Mehrotra R, Singh M, Kumar D. Age specific incidence rate and pathological spectrum of oral cancer in Allahabad. Indian J Med Sci. 2003;57(9):400-4. [Google Scholar]
- Misra V, Singh P, Lal N, Agarwal P, Singh M. Changing pattern of oral cavity lesions and personal habits over a decade: Hospital based record analysis from Allahabad. Indian J Community Med. 2009;34(4):321-5. [Google Scholar] [Crossref]
- Hassawi B, Ali E, Subhe N. Tumours and tumour like lesions of the oral cavity. A study of 303 cases. Tikrit Med J. 2010;16(1):177-83. [Google Scholar]
- Durazzo M, Araujo C, Neto J, Potenza A, Costa P, Takeda F. Clinical and epidemiological features of oral cancer in a medical school teaching hospital from 1994 to 2002: increasing incidence in women, predominance of advanced local disease, and low incidence of neck metastases. Clinics (Sao Paulo). 2005;60(4):293-8. [Google Scholar]
- Bhattacharjee A, Chakraborty A, Purkaystha P. Prevalence of head and neck cancers in the north east—An institutional study. Indian J Otolaryngol Head Neck Surg. 2006;58(1):15-9. [Google Scholar] [Crossref]
How to Cite This Article
Vancouver
Gupta I, Rani R, Suri J. Histopathological spectrum of oral cavity lesions – A tertiary care experience [Internet]. Indian J Pathol Oncol. 2021 [cited 2025 Sep 22];8(3):364-368. Available from: https://doi.org/10.18231/j.ijpo.2021.071
APA
Gupta, I., Rani, R., Suri, J. (2021). Histopathological spectrum of oral cavity lesions – A tertiary care experience. Indian J Pathol Oncol, 8(3), 364-368. https://doi.org/10.18231/j.ijpo.2021.071
MLA
Gupta, Ishani, Rani, Rekha, Suri, Jyotsna. "Histopathological spectrum of oral cavity lesions – A tertiary care experience." Indian J Pathol Oncol, vol. 8, no. 3, 2021, pp. 364-368. https://doi.org/10.18231/j.ijpo.2021.071
Chicago
Gupta, I., Rani, R., Suri, J.. "Histopathological spectrum of oral cavity lesions – A tertiary care experience." Indian J Pathol Oncol 8, no. 3 (2021): 364-368. https://doi.org/10.18231/j.ijpo.2021.071
