- Visibility 79 Views
- Downloads 19 Downloads
- Permissions
- DOI 10.18231/j.ijpo.2020.034
-
CrossMark
- Citation
Solid lesions of pancreas a diagnostic dilemma: Utility of histopathology
- Author Details:
-
Kalaranjini K V
-
Limi Mohandas *
-
Sheela Vasudevan
Abstract
Introduction: Pancreatic pseudotumor: solid non neoplastic lesions of pancreas can often mimic pancreatic cancer clinically and radiologically. Despite major evolution and development in radiology accurate diagnosis of pancreatic lesion are often difficult. The purpose of the study was to assess the diagnostic accuracy of USG in pancreatic lesion and study various solid lesions of pancreas in our tertiary care center.
Materials and Methods: A descriptive study done on all resections (PPPD and Frey excision) of pancreas for a period 18 months. A total of 30 cases were included with adequate clinical and radiological features. Formalin fixed paraffin embedded sections were studied and analysed for USG findings, signs and symptoms, associated co morbidities and histological factors.
Results: Females were more affected than males (1.7:1). Solid lesions presented in individuals as young as 21years to older individuals of 71yrs. The solid lesions included inflammatory lesions (such as acute and chronic pancreatitis) and neoplastic lesions. Most common clinical presentation was jaundice and vague abdominal pain accounting for 67.8 percent of study population. The histomorphological spectrum of solid lesions included 14 cases of inflammatory lesions and 16 cases of neoplastic lesion ([Table 1]). Among the 16 cases neoplastic lesion 5 cases had coexisting tropical pancreatitis. USG examination showed a sensitivity of 53.85%, specificity of 38.46%, positive predictive value of 46.67% and negative predictive value of 45.45% and accuracy of 46.15% for USG examination. Histomorphological features of pancreatitis were studied and most common finding was calcification (100%) present as both microscopic concretions or macroscopic calculi, followed by fatty changes (77%) and fibrosis (72%).
Conclusion: Solid lesions of pancreas still pose diagnostic difficulty for clinician. USG has poor predictive value for non-neoplastic lesions. Histopathological examination remains the gold standard for diagnosis. However, emphasis for minimally invasive techniques such as FNAC must be given.
Introduction
Pancreas is a distinct organ due to its varied function and physiology. An organ formed from two separate buds or anlagen which later rotate and fuse.[1] The organ with its dual composition and function has myriads of role ; with it comes an array of pathology. Pancreas gained its significance from 18th century with advent of Whipple surgery for pancreatic cancer.[2] Around 19th century the endocrine nature of pancreas gained interest with discovery of insulin by Banting.[3]
Diverse lesions of pancreas include inflammatory and neoplastic i.e., from pancreatitis to adenocarcinoma. These lesions often present as solid mass lesions of pancreas. In the age with advancement in imaging technology, innovation in radiology ; fair assessment of pancreatic lesions had led to decreased number of invasive surgeries. Although the advances in imaging increased the discovery of pancreatic masses, their correct identification as a nonneoplastic process is still difficult.[4] Pancreatic pseudotumor do not represent a single entity, but multiple distinct categories of lesions characterised by an enlargement of nonneoplastic character, which clinically resembles a true neoplasm so closely as to often be mistaken for such.[5] Hence the ideal diagnostic (gold standard) test remain histopathological examination.
Aims and Objectives
To study histomorphological spectrum of solid lesions of pancreas.
To assess the usefulness of USG in comparison of histopathology in diagnosing pancreatic pseudotumors.
To assess other coexisting lesions in pancreatic neoplasm
Materials and Methods
A descriptive study done on all resections (PPPD and Frey excision) of pancreas from a period of August 2016 to January 2018 in a tertiary care centre in south India. A total of 30 cases were included. Study was commenced after approval from institutional ethics and research committee. Clinical and radiological features were collected from the patients after appropriate consent. Formalin fixed paraffin embedded sections were cut into 5-micron meter thick section and stained with haematoxylin and eosin. Tumours were classified according to WHO classification appropriate TNM staging was done according to CAP protocol. IHC was done in relevant cases. All data were entered in Microsoft excel and analysed by SPSS software.
Inclusion criteria
All resection cases included with patients above 20 years.
Exclusion criteria
USG guided biopsies were not included
Paediatric (<11years) lesions were not included.
Block resection of abdomen with secondary pancreatic pathology were not included.
Results
Thirty cases of solid lesions of pancreas were studied over a period of 18 months. Demographic factors such as age, sex was included and in our study, females were more affected than males (1.7:1). Solid lesions presented in individuals as young as 21 years to older individuals of 71yrs.
The solid lesions included inflammatory lesions (such as acute and chronic pancreatitis) and neoplastic lesions. Age wise distribution showed difference with respect to lesions. The mean age of inflammatory lesions were 48years and for neoplastic lesions were 62 years. Most common clinical presentation was jaundice and vague abdominal pain accounting for 67.8 percent of study population. Only a single case presented as malena with absence of other symptoms and signs.
The histomorphological spectrum of solid lesions included 14 cases of inflammatory lesions and 17 cases of neoplastic lesion ([Table 1]). Among the 16 cases neoplastic lesion 5 cases had coexisting tropical pancreatitis.
| Nature of lesion | Number of cases |
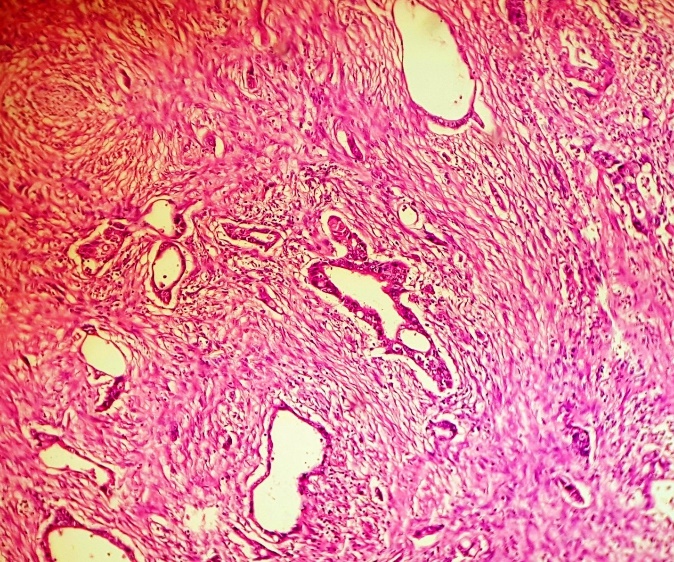
| Pancreatic adenocarcinoma (Figure 1 ) | 12 |
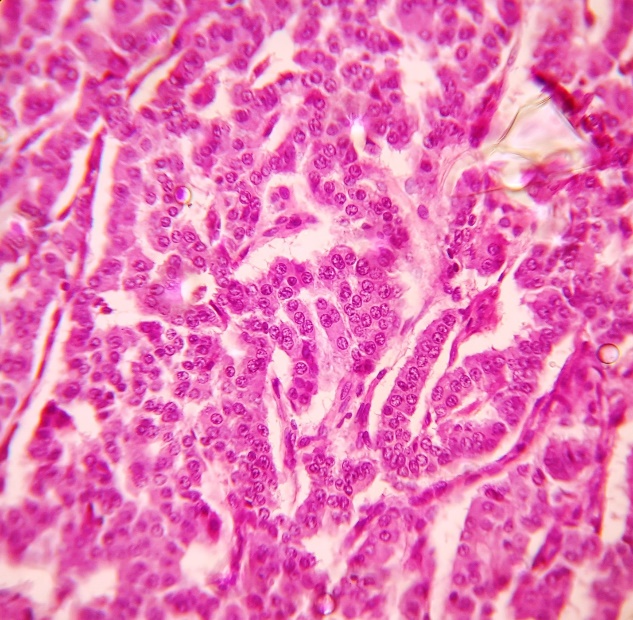
| Pancreatic endocrine tumor (Figure 2 ) | 2 |
| IPMN | 1 |
| Mucinous cystadenoma | 1 |
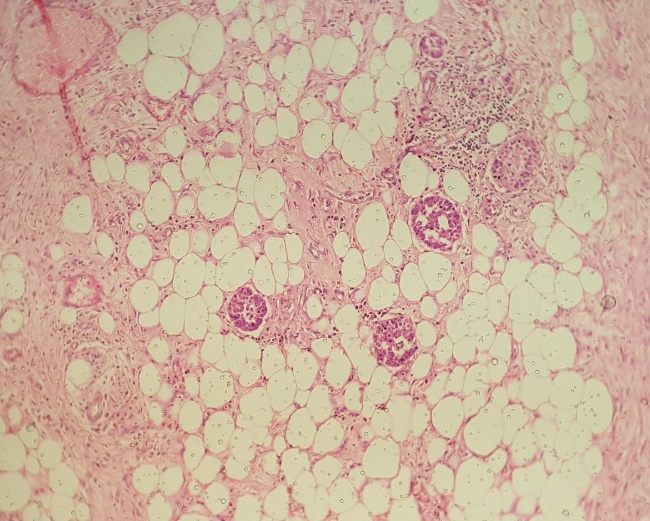
| Chronic pancreatitis (Figure 3 ) | 13 |
| Acute pancreatitis | 1 |
These lesions presented as solid lesions on USG examination, among 16 cases of neoplastic aetiology all cases were shown have positive findings in both USG and histopathology examination. However among 13 cases of chronic pancreatitis proven histologically, 6 cases were diagnosed as neoplastic lesion on USG examination; hereby giving a sensitivity of 53.85%, specificity of 38.46%, positive predictive value of 46.67% and negative predictive value of 45.45% and accuracy of 46.15% for USG examination.
| Radiologically chronic pancreatitis | Histologically proved chronic pancreatitis | False negative cases diagnosed as carcinoma | Total cases of chronic pancreatitis |
| 7 | 13 | 6 | 13 |
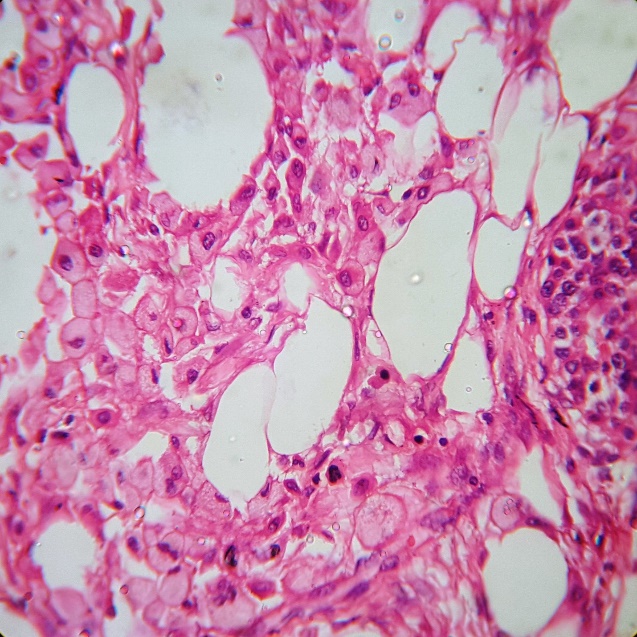
Histomorphological features of pancreatitis were studied and most common finding was calcification (100%) present as both microscopic concretions or macroscopic calculi, followed by fatty changes (77%) and fibrosis (72%). Least common macroscopic finding was pseudocyst formation and fat necrosis ([Figure 4]) accounting for 23%. Microscopic examination showed fatty changes, fibrosis, acinar atrophy and mild chronic inflammation in all cases. Autoimmune pan creatitis was not diagnosed in our study. Only a single case of acute pancreatitis was seen, hence their feature was not statistically significant.
Among the neoplastic lesions of pancreas, most common pathology in our study was pancreatic adeno carcinoma (12/16), followed by neuroendocrine tumour (2/16). Pancreatic adenocarcinoma showed a mean diameter of 39 mm. Most of the lesions were moderately differentiated (91.7%) and 66.7% showed perineural invasion. Microvascular invasion was absent in all cases. Among the 12 cases of adenocarcinoma, 5 cases (41.67%) showed coexisting chronic pancreatitis thereby showing a positive statistical correlation.
| Tumor type | Mean age | Mean diameter (mm) | Lymph node involvement | Perineural invasion | Microvascular invasion |
| Pancreatic adenocarcinoma | 62 | 39 | 2/12 | 8/12 | 0/12 |
| Neuroendocrine tumor | 60 | 21 | 0/2 | 0/2 | 0/2 |
| Mucinous cystadenoma | 48 | 1 | - | - | - |
| Intraductal Papillary mucinous neoplasm | 67 | 35 | 0/1 | 0/1 | 0/1 |
Discussion
Non neoplastic solid mass lesions of pancreas often pose unique diagnostic challenge. Benign lesions often present as solid mass, imaging characteristics of which can be nonspecific and or misleading. It is important to recognise key cytomorphological features to avoid pitfalls and help distinguishing these lesions. [6]
In our study of solid lesions of pancreas females were more affected as compared to Tingsted et al,[7] Thapa et al[8] and Raju et al.[9] Most studies showed male preponderance.
Life style factors such as alcohol consumption and smoking and diet were not included in our variable. Thirty eight percent age of population had history of diabetes mellitus. These thirty eight percent of cases were solid lesions of pancreatic adenocarcinoma with co-existing chronic pancreatitis suggesting an increased of developing pancreatic cancer in long standing comorbidities.[11], [10]
Clinical presentation of the lesions was comparable with Yadav and Kenji et al,[12] which had jaundice and abdominal pain as the most common clinical symptom. These cases had a shorter duration of symptoms which can be attributed to the location of involvement in pancreatic head. This has been illustrated and was comparable with Era B of Salami et al.[13]
Chronic pancreatitis is a chronic inflammatory disease of exocrine pancreas which in comparison with adenocarcinoma has a better prognosis. Often as a part of pre operative diagnosis, imaging analysis of these lesions is done. However the sensitivity and specificity of these modalities has been a question. In our study we observed that the imaging modalities were excellent in detecting neoplastic lesions however often had poor predictive value for non-neoplastic lesion and its delineation from neoplasm ([Table 2]). This lead to inadvertent misdiagnoses and improper management of the patients. This was comparable by Y. Issa et al.[14]
In our study 13/13 case of chronic pancreatitis were of tropical pancreatitis type characterised by gross calculi, fibrosis and fatty change. Balakrishnan et al[15] and Augustine et al[16] had done studies on tropical pancreatitis in south India and found association of cassava intake with tropical pancreatitis. Their study also showed macroscopic features such a calculi formation, fibrosis and fatty change which was corroborating with our study. Microscopic maintenance of lobular pattern even in advanced cases was normal. Preservation of islet and atrophy of acini were found in all cases. However, ductular transformation of acini in the formation of tubular complexes closely packed clusters were seen in single case. Etemadi et al[17] has similar findings of tubular complexes and mild chronic inflammation as seen in our study.
Among the neoplastic lesion pancreatic adenocarcinoma was most common, and worldwide pancreatic ductal carcinoma represents the fourth common cause of death i.e., cancer with a survival rate of less than 1-2%. In our study 41.67 percentage of adenocarcinoma had co existing chronic pancreatitis. Several pathogenic mechanisms have been implicated in the development of pancreatic adenocarcinoma. Among them cationic trypsinogen gene which is present in hereditary chronic pancreatitis has been implicated. In our setup in southern India, tropical pancreatitis is in higher incidence, aetiology of which is still unknown. Irrespective of the underlying aetiology, the continuum of progressive parenchymal destruction, dedifferentiation of acinar into tubular complex, immune cell infiltration and inflammation has known to cause neoplastic transformation. In our study 41.67 percent of cases showed coexisting pathology suggesting a possible link of oncogenic transformation in chronic pancreatitis.
Conclusion
Solid mass lesions of pancreas often pose a unique diagnostic challenge. A variety of non-neoplastic conditions may form pancreatic masses that mimic carcinoma. Approximately 5-10% of pancreatectomies performed with clinical diagnoses of pancreatic cancer prove to be pseudotumor on microscopic examination. Imaging advances has not helped in replacing histopathology as gold standard for proper delineation of nature of these lesions. However, emphasis for minimally invasive techniques such as FNAC must be given in the upcoming era.
Source of funding
None.
Conflict of interest
None.
References
- Abraham S, Wilentz R, Yeo C, Sohn T, Cameron J, Boitnott J. Whipple Resections) in Patients Without Malignancy. Am J Surg Pathol. 2003;27(1):110-120. [Google Scholar]
- Fernandez-Del Castillo C, Morales-Oyarvide V, Mcgrath D. Evolution of the Whipple procedure at the Massachusetts General Hospital. Surg. 2012;152:56-63. [Google Scholar]
- Banting F, Best C. The Discovery and Preparation of Insulin. Univ Toronto Med J. 2010;87(3). [Google Scholar]
- Zamborini G, Paola C, . AS. Non neoplastic mimickers of pancreatic neoplasms. Arch Pathol Lab Med. 2009;133(3):439-453. [Google Scholar]
- Adsay NV, Baslik DS, Klimstra -. Pancreatic pseudotumor: non neoplastic solid lesions of the pancreas that clinically mimic pancreas carcinoma. Semin Diagn Pathol. 2004;21:260-267. [Google Scholar]
- Tingstedt B, Weitkamper C, Andersson R. Early onset pancreatic cancer: a controlled trial. Ann Gastroenterol. 2011;24(3):206-212. [Google Scholar]
- Raju RS, Coburn N, Liu N, Porter JM, Seung SJ, Cheung MC, et al. A population-based study of the epidemiology of pancreatic cancer: A brief report. Curr Oncol. 2015;22:478-478. [Google Scholar]
- Thapa P. Epidemiology of Pancreatic and Periampullary Cancer. Indian J Surg. 2015;77(5):358-361. [Google Scholar]
- Ben Q, Xu M, Ning X. Diabetes mellitus and risk of pancreatic cancer: a meta-analysis of cohort studies. Eur J Cancer. 2011;47(13):1928-1937. [Google Scholar]
- Li D, Tang H, Hassan MM, Holly EA, Bracci PM, Silverman DT. Diabetes and risk of pancreatic cancer: a pooled analysis of three large case-control studies. Cancer Causes Control. 2011;22(2):189-1897. [Google Scholar]
- Yadav D, Notahara K, Smyrk TC, Clain JE, Pearson RK, Farnell MB, et al. Idiopathic tumefactive chronic pancreatitis: clinical profile, histology, and natural history after resection. Clin Gastroenterol Hepatol. 2003;1:129-135. [Google Scholar]
- Salami A, Obaid T, Joshi AR. Trends in the clinical presentation, treatment, and survival for pancreatic adenocarcinoma. Am J Surg. 2019;217(1):103-107. [Google Scholar]
- Issa Y, Kempeneers MA, Van Santvoort HC. Diagnostic performance of imaging modalities in chronic pancreatitis: a systematic review and meta-analysis. Eur Radiol. 2017;27:3820-3864. [Google Scholar]
- Balakrishnan V, Nair P, Radhakrishnan L, Narayanan VA. Tropical pancreatitis - a distinct entity, or merely a type of chronic pancreatitis?. Indian J Gastroenterol. 2006;25(2):74-81. [Google Scholar]
- Augustine P, Ramesh H. Is tropical pancreatitis premalignant?. Am J Gastroenterol. 1992;87:1005-1008. [Google Scholar]
- Etemad B, Whitcomb DC. Chronic pancreatitis: diagnosis, classification, and new genetic developments. Gastroenterol. 2001;120:682-707. [Google Scholar]
- Shrikhande SV, Barreto G, Koliopanos A. Pancreatic carcinogenesis: the impact of chronic pancreatitis and its clinical relevance. Indian J Cancer. 2009;46:288-296. [Google Scholar]
How to Cite This Article
Vancouver
V KK, Mohandas L, Vasudevan S. Solid lesions of pancreas a diagnostic dilemma: Utility of histopathology [Internet]. Indian J Pathol Oncol. 2020 [cited 2025 Sep 22];7(1):181-185. Available from: https://doi.org/10.18231/j.ijpo.2020.034
APA
V, K. K., Mohandas, L., Vasudevan, S. (2020). Solid lesions of pancreas a diagnostic dilemma: Utility of histopathology. Indian J Pathol Oncol, 7(1), 181-185. https://doi.org/10.18231/j.ijpo.2020.034
MLA
V, Kalaranjini K, Mohandas, Limi, Vasudevan, Sheela. "Solid lesions of pancreas a diagnostic dilemma: Utility of histopathology." Indian J Pathol Oncol, vol. 7, no. 1, 2020, pp. 181-185. https://doi.org/10.18231/j.ijpo.2020.034
Chicago
V, K. K., Mohandas, L., Vasudevan, S.. "Solid lesions of pancreas a diagnostic dilemma: Utility of histopathology." Indian J Pathol Oncol 7, no. 1 (2020): 181-185. https://doi.org/10.18231/j.ijpo.2020.034
