- Visibility 109 Views
- Downloads 25 Downloads
- DOI 10.18231/j.ijpo.2024.063
-
CrossMark
- Citation
A case of inflammatory myofibroblastic tumor of small intestine, presented as intussusception
- Author Details:
-
Keerthana Muppidi *
-
Takkalapally Prasanna Vaibhav
Introduction
Inflammatory myofibroblastic tumor (IMT) is a very rare tumor that has been considered a soft tissue neoplasm of intermediate biological potential with a low risk of recurrence and metastasis to other sites.[1]
Inflammatory myofibroblastic tumors can occur in multiple sites. The descending order of occurrence is lung, followed by intra-abdominal organs like the liver, spleen, and mesentery. Small bowel tumors are extremely rare. The most common clinical symptoms of an inflammatory myofibroblastic tumor involving the intra-abdominal organs are pain abdomen and alteration in bowel habits.[2]
The most characteristic histopathological features of an IMT are spindle cell proliferation, arranged in a fascitis-like manner with areas of myxoid change and collagenous background. Hypocellular areas are also seen.[3] Several mixed inflammatory cell infiltrates are seen consisting of mainly plasma cells, lymphocytes, and eosinophils, and few neutrophils and foamy macrophages are seen rarely.[4]
Case Presentation
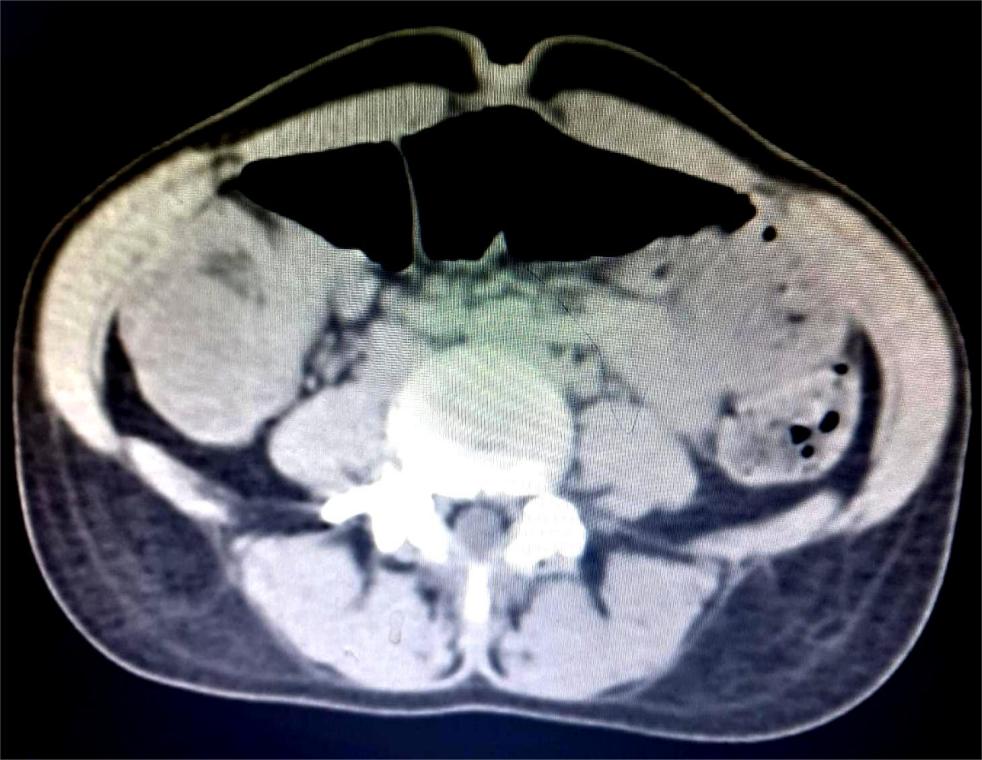
This is a case of 23-year-old female who came to the surgical outpatient with chief complaints of pain in the abdomen, constipation, and bleeding per rectum. Per abdominal examination showed soft, non-tender, and no organomegaly. There is slight abdominal distension. Routine investigations and viral screening were done. A complete blood picture showed moderate anemia (Hb - 8.0 g/dl) and neutrophilic leucocytosis (WBC count - 16,800 cells/ cu mm and 78% neutrophils). X-ray showed dilated bowel loops. The patient is admitted immediately. Ultrasound abdomen was advised. It showed a bowel within bowel appearance measuring 4x3.6 cm, noted in the right iliac fossa region, and a diagnosis of? Intussusception (ileocolic) given. Later contrast enhanced computed tomography (CECT) abdomen was done which showed intussusception of the ileum into the caecum with proximal terminal ileal loop dilatation. There is slight contrast enhancement suggesting a mass of 3x2 cm in size. The patient was posted for exploratory laparotomy and the ileocaecal segment was excised followed by end-to-end anastomosis. Post-surgery is uneventful. The specimen has been received in the pathology department for histopathological examination. A gross examination was done which showed an already cut opened segment of the small intestine measuring 10 cm in length. Lumen showed an attached polyp measuring 3x2x1.5 cm. The cut section of poly is solid, grey-white. Microscopic examination showed an ill-defined tumor at the level of the submucosa, just below the muscularis mucosae. Spindle-shaped cells were seen having eosinophilic cytoplasm and spindle-to-oval vesicular nuclei. Prominent inflammatory infiltrates are seen consisting of lymphocytes, plasma cells, eosinophils, and a few neutrophils. Areas of hypocellularity and myxoid change were seen. There is no significant mitotic activity and no areas of necrosis. Overlying small intestinal mucosa showed foci of ulceration and granulation tissue. Based on the typical microscopic features diagnosis of inflammatory myofibroblastic tumor was made. Inflammatory fibroid polyp was considered as the diffential diagnosis. Advised IHC (immunohistochemistry) study with Smooth muscle actin (SMA), CD34 (cluster differentiation), and Anaplastic lymphoma kinase (ALK) for confirmation.



Discussion
Inflammatory myofibroblastic tumors were previously called inflammatory pseudotumor, inflammatory fibrosarcoma, and plasma cell granuloma because of plenty of inflammatory infiltrates consisting of mainly mature plasma cells and lymphocytes. But their terms are obsolete now. This tumor can occur both in children and in adults. However small intestinal mesenteric inflammatory myofibroblastic tumor is common in preadolescent children. The cause of this tumor was not understood fully till today.[5] Literature says that the occurrence of tumors is associated with gastric ulcers, chronic gastritis, ischaemic conditions, and the use of certain drugs like nonsteroidal anti-inflammatory drugs. Abnormalities involving chromosomal locus 2p23 are present in the most of the cases of IMT. Genetic abnormalities that occur result in the formation of the ALK (anaplastic lymphoma kinase), a fusion protein that is a potent growth factor receptor. Approximately 60 percent of inflammatory myofibroblastic tumors have gene rearrangements and the interesting part is, it is more common in patients younger than 10 years of age. [6] About 5% of IMTs have ROS1(ROS proto-oncogene 1, receptor tyrosine kinase) gene fusions. DNA aneuploidy and association with some oncogenic viruses like Epstain-Barr virus (EBV), and Human Herpes virus type 8 (HHV 8) have been demonstrated to be the pathogenesis of IMT by some investigators. Even over-expression of Interleukin-6 is proposed to be involved in the pathogenesis of the tumor. [4] However, the exact pathogenesis of the tumor is not clear still. [7]
Presenting symptoms depend on the involved primary site by the tumor. The lung is the most affected site, but extra pulmonary IMT may include the mesentery-omentum, upper respiratory tract, genitourinary tract, retro peritoneum, pelvis, head, neck, spleen, brain, pancreas, liver, and gastrointestinal tract.[8] This tumor rarely emerges in the small intestine, and there are a few patients with intestinal manifestations.[9]
In the present case, as shown in ([Figure 1]), on contrast enhanced computed tomography there is telescoping of small intestinal loop into to the small bowel loop. The tumor is seen arising from the terminal ileum at the level of submucosa and the patient presented with intussusception. Intussusception is defined as the telescoping of the proximal segment of the intestine within the lumen of the adjacent distal segment of the intestine. Intussusception is rare in adults when compared to its occurrence in children. The incidence of intussusception is two to three cases per population of 1,000,000 per year. [10]
Inflammatory myofibroblastic tumors on gross are typically seen as solid grey-white lesions with infiltrative borders. Few show foci of myxoid change.
As shown in ([Figure 2] A,B), in the present case a 3x2 cm polypoidal mass with broad base and outer surface showing hemorrhagic areas is seen arising from the small intestine. Microscopic examination showed, under scanner and low power poorly circumscribed lesion located below muscularis propria with spindle-shaped cells arranged in loose fascicles. High power examination under the microscope showed spindle-shaped cells with features of myofibroblasts, plenty of inflammatory infiltrates mainly mature plasma cells, small lymphocytes, and few eosinophils.
([Figure 3]) shows that the tumor is located at the level of the submucosa of the ileum. ([Figure 4]) shows the typical proliferation of myofibroblasts against a myxoid background mixed with plasma cells and a few eosinophils.
Immunohistochemically the tumor cells in IMT are generally positive for Smooth muscle actin (SMA), desmin, and anaplastic lymphoma kinase (ALK). Also, a positive reaction is seen with other markers like vimentin and muscle-specific actin. Tumors may also be focally positive for CD34 and factor XIIIa.[7]
The diagnosis IMT was made based on the typical gross and microscopic features on Haematoxylin and eosin staining. IHC was not done in this case which is the drawback of the present case report.
Conclusion
Histopathological examination remains the gold standard for diagnosis of such cases presenting with intestinal obstruction. Small intestinal inflammatory myofibroblastic tumors are very rare, so presenting this case report.
Sources of Funding
None.
Conflict of Interest
None.
References
- L Gros, APD Tos, RL Jones, A Digklia. Inflammatory Myofibroblastic Tumour: State of the Art. Cancers (Basel) 2022. [Google Scholar]
- Anatoly Budylev, Irit Solar, Rivka Kessner. . Asaf Aizic; ROS1-positive Inflammatory Myofibroblastic Tumor of the Small Bowel Causing Obstruction: A Case Report.Radiology Case 2022. [Google Scholar]
- B Gleason, J Hornick. Inflammatory myofibroblastic tumors: where are we now?. J Clin Pathol 2008. [Google Scholar]
- Maryam Rezaii Salim, Homayoon Vahedi1, Zia Salimi, Hossein Froutan. Masoud Sotoudeh; Inflammatory Myofibroblastic Tumor of the Small Bowel: A Case Report. Middle East Journal of Digestive Diseases 2011. [Google Scholar]
- A Oeconomopoulou, YD Verney, K Kanavaki, K Stefanaki, K Pavlakis, C Salakos. Inflammatory myofibroblastic tumor of the small intestine mimicking acute appendicitis: a case report and review of the literature. J Med Case Rep 2016. [Google Scholar]
- RD Odze, JR Goldblum. . Surgical pathology of the GI tract, liver, biliary tract, and pancreas 2009. [Google Scholar]
- YÇ Appak, GE Sahin, S Ayhan, C Taneli, E Kasrga. Inflammatory myofibroblastic tumor of the colon with an unusual presentation of intestinal intussusception. Eur J Pediatr Surg Rep 2014. [Google Scholar]
- A Koyuncuer. Inflammatory myofibroblastic tumor of the small-bowel mesentery: A case report of nonspecific clinical presentation and a review of the literature. Int J Surg Case Rep 2014. [Google Scholar]
- A Amouei, F Ehsani, M Vaghefi, SM Tabatabai, PY Anari. Inflammatory myofibroblastic tumor of the small intestine: A case report. Int J Surg Case Rep 2016. [Google Scholar]
- M Farhan, A Bibi, O Zulfiqar. Adult Mid Ileo-Ileal Intussusception Secondary to Inflammatory Myofibroblastic Tumor (IMT): A Case Report and Literature Review. Cureus 2020. [Google Scholar]
How to Cite This Article
Vancouver
Muppidi K, Vaibhav TP. A case of inflammatory myofibroblastic tumor of small intestine, presented as intussusception [Internet]. Indian J Pathol Oncol. 2024 [cited 2025 Sep 10];11(3):295-298. Available from: https://doi.org/10.18231/j.ijpo.2024.063
APA
Muppidi, K., Vaibhav, T. P. (2024). A case of inflammatory myofibroblastic tumor of small intestine, presented as intussusception. Indian J Pathol Oncol, 11(3), 295-298. https://doi.org/10.18231/j.ijpo.2024.063
MLA
Muppidi, Keerthana, Vaibhav, Takkalapally Prasanna. "A case of inflammatory myofibroblastic tumor of small intestine, presented as intussusception." Indian J Pathol Oncol, vol. 11, no. 3, 2024, pp. 295-298. https://doi.org/10.18231/j.ijpo.2024.063
Chicago
Muppidi, K., Vaibhav, T. P.. "A case of inflammatory myofibroblastic tumor of small intestine, presented as intussusception." Indian J Pathol Oncol 11, no. 3 (2024): 295-298. https://doi.org/10.18231/j.ijpo.2024.063
