Introduction
Invasive papillary carcinoma of the breast is a rare condition.1 This includes less than 1% of all invasive breast cancers. These tumors have a better prognosis when compared with other invasive breast cancer, having lower mortality rate.2 The tumor is present as pain less retroareolar lump or many times with blood in discharge. Even though the frequency of axillary node involvement is low, treatment often involves mastectomy and axillary node dissection.
On histopathogical examination, these tumors present with papillae like growth pattern supported by fibrovascular stalks.3 These tumors are characterized by the presence of areas showing stromal invasion or invasion into lymphovascular spaces. Ultimately, the histopathological examination along with immuno-histochemistry confirms the diagnosis.4 In this, our index case, the patient presented with a lump in the left breast and was diagnosed as a benign fibroadenoma with papillary proliferation after immunohistochemistry in the preoperative period. On post operative histopathological examination, it turned out to be invasive solid papillary carcinoma of the breast. We present this rare type of breast tumor having diagnosis difficulties in the preoperative period.
Case Report
A 55-year-old-menopausal woman presented to the hospital complaining of a left breast retroareolar painless lump for 2 months. She did not have any history of nipple discharge or nipple retraction. Family history was non significant. On clinical examination, an oblong mass was palpable in the retroareolar region of the left breast extending periphery. No nipple retraction or nipple discharge. Examination of the left axilla revealed palpable lymphnodes. The right breast and right axilla were normal on clinical examination.
On bilateral breast mammography, there was a heterogeneous dense breast with an irregular, high-density mass having an oblong component noted in the retro areolar region in the center-left breast involving anterior and middle depth with an indistinct margin (Figure 1). No intra-mass calcification, skin thickening or nipple retraction were seen. Non-specific normal-sized lymph nodes are present in the left axilla. Preoperative ultrasound showed irregular solid and cystic mass lesion in the retroareolar region with a solid component that has high vascularity with surrounding some dilated ducts. Ultrasound guided tissue biopsy from the solid component of mass was done. It was revealed atypical papillary proliferation with underlying Fibroadenoma. The preoperative diagnosis was confirmed by immunohistochemistry. With this pre-operative diagnosis, we did a lumpectomy of the left breast without axillary clearance.
On post-operative histopathological examination, it came out as an invasive solid papillary carcinoma with ductal in situ. Histopathological examination reveled that multiple foci of dilated ducts with papillary fronds comprising of mainly epithelial cell populations. The myoepithelial cells in these papillae appear inconspicuous. We did Immunohistochemistry showed negative stain for myoepithelail cells suggestive invasive papillary carcinoma breast. We did left side modified radical mastectomy with axillary clearance as a second surgery (Figure 1).
Post operative course was uneventful. On postoperative histopathalogical examination (Figure 2) it came out a Invasive solid papillary carcinoma with intra ductal papillary ductal carcinoma in situ of left breast.
Figure 1
(A & B) a heterogeneous dense breast with an irregular, high-density mass having oblong component noted in retroareolar region in the center-left breast involving anterior and middle depth with indistinct margin. (C & D) Intra-operative picture after modified radical mastectomy with axillary clearance and showing thoracodorsal bundle preserved with axillary lymph node dissection
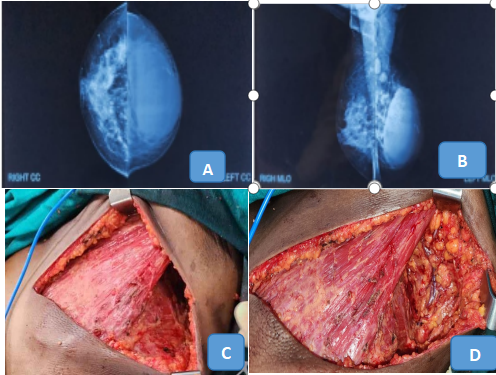
Figure 2
Solid papillary carcinoma with the predominant solid areas with focal papillary pattern of neoplastic cells (★) (A, HE, 50X). Solid cellular epithelial nodules are separated by thin, delicate fibrovascular septa (B, HE, 100X). Perivascular rosettes and the neoplasticcells show monotonous hyperchronatic nuclei with inconspicuous mitosis (C, HE,100X). Nests of sebaceous metaplastic cells are seen admixed with neoplastic cells (◆) (D, HE, 100X). Adjacent to the lesion, papillary DCIS areas are seen (E, HE, 50X). Dilated ducts filled with slender papillary fronds having find fibrovascular stalks covered by neoplastic epithelial cells of intermediate nuclear grade with inconspicuous myoepithelial cells (F, PAS, 50X)

Discussion
Papillary carcinomas of breast are a very rare type of invasive tumor. These tumors are present in the post-menopause age group of women.5 Papillary neoplasms of breast can present with different clinical and radiological features.
As in our index case, the preoperative core needle biopsy showed a fibroadenoma with papillary configuration and later it came out as a papillary invasive carcinoma on the post-operative histopathological examination. Immunohistochemistry has a main role in confirming the diagnosis.
Papillary invasive carcinomas, clinically, can present asymptomatic, or can present with bloody nipple discharge or painless retroareolar mass as presented in our index case.6 Malignant papillary neoplasm of the breast includes several types of microscopically distinct lesions such as DCIS (Ductal Carcinoma in Situ) arising in intraductal papilloma, papillary DCIS, encapsulated papillary carcinoma, solid papillary carcinoma, and invasive papillary carcinoma.7 All malignant papillary lesions of the breast lack an intact myoepithelial cell layer (MCL) within the papillae or at the periphery of the tumor.
Mammography can show a round, oval or irregular high-density mass, sometimes associated with satellite nodules, and margins are circumscribed but may be obscured or indistinct.8 Along with findings, microcalcification or a dilated ductal pattern may be present in distinct types of lesions.9 On ultrasonography, these tumors present like a hypoechoic mass with a posterior acoustic shadow. These tumors can present with a complex structure having both cystic as well as solid components with increased vascularity.10 The Image guided tissue biopsy has more role in the exact tissue diagnosis as compared with non-guided biopsy.
Immunohistochemistry has main role in the diagnosis of this condition. The myoepithelial cells and basement membrane are absent in this types of tumors. In the invasive tumors myoepithelial cells are absent.11 There are many mayoepithelial markers like S-100, Calponin, CD 1O, smooth muscle myosin heavy chain, alpha-smooth muscle actin, P63, and high molecular weight Cytokeratin with different sensitivities and specificity.12 Out of these markers P63 and smooth muscle, myosin is more specific. The P63 myoepithelial marker stains only in cell muscles. Some chromosomal abnormalities also associated with this condition. Loss of heterozygosity (LOH) of 16q23 is specific to the malignant lesion.
Treatment options are wide local excision, with or without adjuvant radiotherapy or chemotherapy.13
Conclusion
Even though invasive papillary carcinoma breast is a rare variety, it carries an excellent prognosis, but preoperative correct diagnosis remains challenging. Sometimes it mimics as a benign condition. Thorough preoperative clinical and radio-logical examination should be done, so that timely management as well as proper treatment is possible.
Consent
We have taken the valid informed consent from the patient as well as her son for publication.
Source of Funding
All authors have declared that no financial support was received from any organization for the submitted work.
