- Visibility 113 Views
- Downloads 21 Downloads
- DOI 10.18231/j.ijpo.2023.027
-
CrossMark
- Citation
A histopathological study of ovarian lesions in a rural medical college
- Author Details:
-
Qureshi Saba Yasmeen
-
Sheetal Mahajan Dhule *
-
Piyush Prakash Narkhede
-
Tooba Fatima Mohammed Shafee
-
Ishrath Fatema
Introduction
Ovarian lesions have a broad spectrum of presentation in clinical practice. Therefore, it is important to know there histological diagnosis for management. Also, on clinical examination, most of the non neoplastic lesions forming pelvic mass mimic ovarian neoplasm. The purpose of the study was to analyze the spectrum of ovarian lesions in a tertiary care centre and to categorize histomorphological pattern as non neoplastic, benign, borderline and malignant.
The ovaries are paired organs located on the sides of the uterus close to the lateral pelvic wall, behind the broad ligament and anterior to the rectum.[1] Most commonly lesions encountered in the ovary are functional or benign cysts and tumors. Oophoritis are uncommon and in rare occasion autoimmune pathology can arise in ovary.
Non-neoplastic and functional cysts include follicle cyst, luteal cyst, polycystic ovaries and stromal hyperthecosis. Cystic follicles are very common in the ovary. Functional cysts differ from neoplastic cysts in being usually of size 6-8cm, asymptomatic, regress spontaneously and are unilocular containing clear fluid.[2] These are frequently seen in young female in their 2 decade due to failure of ovulation. Ovarian cysts usually present with pain or discomfort in lower abdomen. Cyst rupture may lead to peritoneal signs, abdominal distention.[3], [4] Polycystic ovarian syndrome also known as Stein Leventhal syndrome, affects 6% to 10% of reproductive age group women worldwide. Association with obesity, type 2 diabetes and premature atherosclerosis is there.
In ovary neoplastic lesions can be grouped according to their origin from each of the three main types; mullerian epithelium, germ cells and sex cord stromal cells.[5] Ovarian tumors are of numerous types. About 80% are benign. Occurs mostly in between 20 and 45 years of age. Borderline tumors occurs at slightly older ages. Malignant tumors are more common in women between 45 and 65 years of age. Ovarian tumors are called as silent killers as they are difficult to detect until they are advanced in size or stage.[6] Also ovaries are inaccessible therefore easy screening methods are not available.[7] Ovarian cancer comprises up to 8.7% of cancers in different parts of India.[8], [9] Ovarian cancer accounts for 3% of all cancers in females in the United states. Epithelial ovarian tumors are classified into benign, borderline and malignant. Majority of the malignant epithelial tumors are high grade serous carcinoma. They have poor prognosis as are detected after they have spread beyond the ovary and fallopian tube.
Materials and Methods
This was a observational, cross-sectional study done between January to December 2022 in department of Pathology of JIIU’s IIMSR, Warudi, in Jalna district of Maharashtra. Approval of Institutional ethical committee was obtained for this study. The histopathological specimen of the patients who underwent ovarian resection and total abdominal hysterectomy with bilateral salphingo-oophorectomy were included in the study. Total 132 samples were received in our department. Specimens were fixed in 10% formalin. Relevant clinical details were obtained from the medical records. Detailed gross finding were noted and representative section submitted. The tissue was processed in fully automated processing unit, blocks prepared, 3-5 microns tissue sections were cut by Leica microtome and the sections were stained with Haematoxylin and Eosin stain. Slides were reported by atleast two pathologists and histopathological diagnosis was finalized. The details of the patients and data were kept confidential. The data was analysed using MS Excel worksheet.
Results
A total of 132 cases of ovarian lesions were included in this study. The patients were in the age range of 20 to 72 years of age.
|
S. No |
Age wise categories |
Non neoplastic |
Neoplastic |
|
||
|
Benign |
Malignant |
Borderline |
Total |
|||
|
1 |
20-29 years |
2 |
15 |
|
|
17 (12.88%) |
|
2 |
30-39years |
25 |
24 |
1 |
2 |
52 (39.40%) |
|
3 |
40-49years |
34 |
12 |
|
1 |
47 (35.6%) |
|
4 |
50-59years |
6 |
2 |
|
|
8 (6.06%) |
|
5 |
>60years |
4 |
3 |
1 |
|
8 (6.06%) |
|
|
Total |
71 |
56 |
2 |
3 |
132 |
Upto 29 years benign neoplastic lesions were the commonest. After 30 years majority of the lesions were non neoplastic.([Table 1])

The non neoplastic lesions constituted 54% (71 out of 132) of the total cases.

Follicular cysts were the commonest amongst the non neoplastic lesions (48 out of 71 cases).

Mucinous cyst adenoma were the commonest amongst the neoplastic lesions (20 out 61 cases) followed by serous cyst adenoma (18 out of 61 cases).
|
Category |
Histopathological Diagnosis |
Unilateral |
Bilateral |
|
Non - neoplastic |
|
|
|
|
|
Follicular cyst |
34 |
14 |
|
|
Endometriosis |
3 |
|
|
|
Haemorhagic luteal cyst |
16 |
|
|
|
Haemorhagic cysts |
4 |
|
|
Neoplastic |
|
|
|
|
Benign |
Mucinous cyst adenoma |
19 |
1 |
|
|
Serous cyst adenoma |
17 |
1 |
|
|
Mature cystic Teratoma |
15 |
|
|
|
Fibro thecoma |
2 |
|
|
|
Ovarian fibroma |
1 |
|
|
Malignant |
Papillary serous cyst adenocarcinoma |
2 |
|
|
Borderline |
Mucinous neoplasia |
2 |
|
|
Serous neoplasia |
1 |
|
|
|
Total |
132 |
116 |
16 |
Majority of ovarian lesions presented as unilateral lesions - 87.87% (116 out of 132 cases).


Discussion
In our study 132 cases of ovarian lesions were included. Most of the cases presented in 3rd and 4th decade of life. Study done by Purti Agrawal et al[10] had peak incidence of ovarian tumor in 3rd and 5th decade of life. In our study majority of the ovarian lesions were unilateral (116/132 cases) 87.87%. Bilateral ovarian lesions were 12.12% which was in concordance with studies done by Maitry D Charel et al,[11] Couto et al. [12]
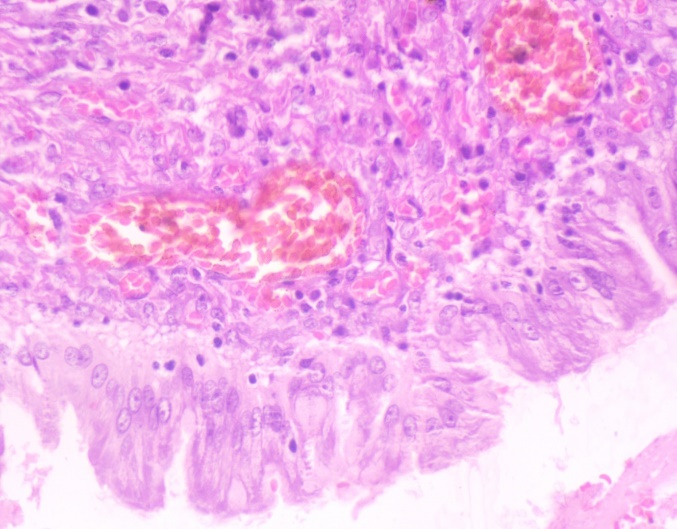
Non neoplastic lesions were 71/132 cases (53.78%) and neoplastic lesions were 61/132 cases (46.22%). Similar findings were seen in studies done by Nehal Ahmad et al[13] non neoplastic 55.8% and neoplastic 44.2%. The most common non neoplastic lesion was follicular cyst (48/71 cases) followed by haemorrhagic luteal cyst. Studies done by Amod Sawant et al,[14] Thakkar et al[15] had similar findings. Ashraf et al[16] had corpus luteal cyst as the commonest non neoplastic lesion.
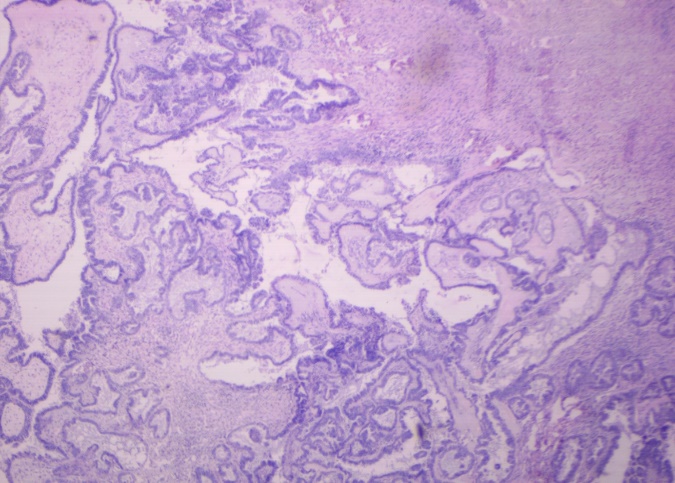
Commonest neoplastic lesion encountered in present study was mucinous cyst adenoma (32.78%) which was in concordance with study done by Purti Agrawal et al.[10] Mondal et al. had serous cystadenoma (32.57%) as the most commonest histiologic type followed by mucinous cyst adenoma (15.71%).
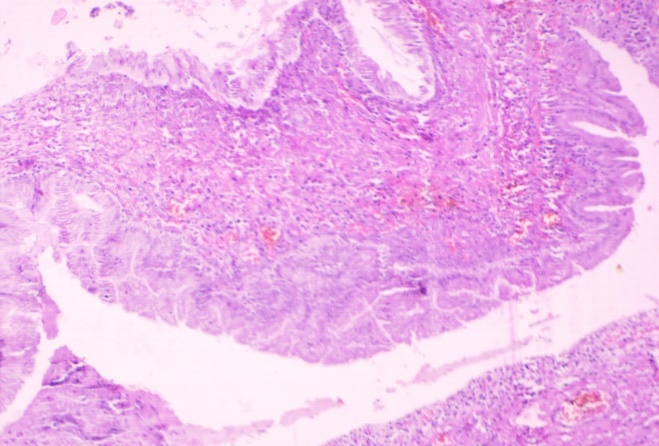
In borderline cases, two cases were of mucinous cyst adenoma borderline and one case of serous cyst adenoma borderline. In studies done by Agrawal et al and Bhagyalaxmi et al[17] most common borderline ovarian tumor was borderline mucinous tumor 55.5%. Two cases turned out to be malignant both being serous cyst adenocarcinoma. Amongst the malignant epithelial tumors, serous cyst adenocarcinoma was the commonest in study done by Maheshwari et al.[18]
Ovarian lesions contribute major proportion of the cases of abdominal and pelvic swellings in female population. The prevalence of various ovarian pathologies varies according to age. Radiological investigations like transvaginal ultrasonography and CT scan helps in accessing size, spread and probable diagnosis of ovarian lesions. Many studies concluded that grossly most of non neoplastic and neoplastic ovarian lesions present as cystic swellings; while malignant and borderline lesions are partly solid and partly cystic. However, HPE confirmation always remains the gold standard for the diagnosis. It also helps in clinical staging and appropriate management of the patients.
Conclusion
Ovarian lesions are common in younger age group. Most of the cystic lesions of ovary are asymptomatic. In present study, follicular cyst was most common diagnosis amongst the non neoplastic lesions of ovary. Borderline mucinous cystadenoma was the commonest in borderline cases and in malignant cases serous cystadenocarcinoma was the commonest. Hence histopathological examination of ovarian lesions is important for exact diagnosis and proper management.
Source of Funding
None.
Conflicts of Interest
There are no conflicts of interest.
References
- JR Goldblum, LW Lamps, JK McKenney, JL Myers, B Gilks. Ovary. Rosai and Ackerman’s Surgical Pathology 2018. [Google Scholar]
- H Konar. . Textbook of Gynecology 2013. [Google Scholar]
- C Bottomley, T Bourne. Diagnosis and management of ovarian cyst accidents. Best Pract Res Clin Obstet Gynaecol 2009. [Google Scholar]
- . Practice Bulletin No. 174: Evaluation and Management of Adnexal Masses. Obstet Gynecol 2016. [Google Scholar]
- V Kumar, A Abbas, JC Aster, LH Ellenson, EC Pirog. The Female Genital Tract. Robbins & Cotran Pathologic Basis of Disease 2021. [Google Scholar]
- PD Dhende, LY Patil, K Jashnani. Spectrum of ovarian tumors in a tertiary care hospital. Indian J Pathol Oncol 2021. [Google Scholar]
- PC Smita, AP Anagha, SM Vilas, MD Runali. Clinicopathological Study of Ovarian Lesions. Indian J Pathol Res Pract 2017. [Google Scholar]
- P Basu, P De, S Mandal, K Ray, J Biswas. Study of ‘patterns of care’ of ovarian cancer patients in a specialized cancer institute in Kolkatta, eastern India. Indian J Cancer 2009. [Google Scholar]
- SK Mondal, R Banyopadhyay, DR Nag, S Roychowdhury, PK Mondal, SK Sinha. Histologic pattern, bilaterality and clinical evaluation of 957 ovarian neoplasms: A 10-year study in a tertiary hospital of eastern India. J Cancer Res Ther 2011. [Google Scholar]
- P Agrawal, DG Kulkarni, PR Chakrabarti, S Chourasia, M Dixit, K Gupta. Clinicopathological Spectrum of Ovarian Tumors: A 5 Year Experience in a Tertiary Health Care Center. J Basic Clin Reprod Sci 2015. [Google Scholar]
- MD Charel, SA Shah, HM Goswami. Histopathological Study of Ovarian Cystic Lesions at a Tertiary Care Hospital in India. Int J Contemp Pathol 2020. [Google Scholar]
- F Couto, NS Nadkarni, MJ Rebello. Ovarian tumors in Goa: A clinicopathological study. J Obstet Gynecol India 1993. [Google Scholar]
- N Ahmad, MJ Hassan, S Khan, ZS Jairajpuri, S Jetley. Histopathological Spectrum of Ovarian Lesion in a Tertiary Care Hospital over a Period of Five years. Saudi J Pathol Microbiol 2019. [Google Scholar]
- A Sawant, S Mahajan. Histopathological Study of Ovarian Lesions at a Tertiary Health Care Institute. MVP J Med Sci 2017. [Google Scholar]
- NN Thakkar, SN Shah. Histopathological Study of Ovarian Lesion. Int J Sci Res 2015. [Google Scholar]
- A Ashraf, AS Shaikh, A Ishfaq, A Akram, F Kamal, N Ahmad. The relative frequency and histopathological patterns of ovarian masses. Biomed 2012. [Google Scholar]
- A Bhagyalakshmi, A Sreelekha, S Sridevi, J Chandralekha, G Parvathi, A Venkatalakshmi. Prospective study of histopathological patterns of ovarian tumours in a tertiary care centre. Int J Res Med Sci 2014. [Google Scholar]
- V Maheshwari, SP Tyagi, K Saxena, N Tyagi, R Sharma, M Aziz. Surface epithelial tumors of the ovary. Indian J Pathol Microbiol 1994. [Google Scholar]
