Introduction
Endometrial osseous metaplasia/ osseous material within the uterus is defined as presence of bone (mature or immature) embedded within the endometrium. It is an unusual clinical condition which can be symptomatic or asymptomatic and incidentally detected on ultrasound or gynaecological procedures. Etiopathogenesis is not clear but various theoretical hypotheses have been proposed and studied to explain osseous metaplasia for the presence of bone within the endometrial tissue. This condition is very rare, and its reported incidence is low. Clinically the patients may be asymptomatic or may present with infertility, abnormal uterine bleeding, or lower abdominal pain due to associated pelvic inflammatory disease. Recognition of osseous material within the endometrial cavity as a benign entity is important to avoid misdiagnosis as Carcinosarcoma microscopically, however complete clinicopathological correlation ensures correct diagnosis. The most common association is history of retained fetal products however very few cases have been reported without the history of abortion, here we present such a rare case with an unusual finding of extramedullary hematopoiesis and a brief review of literature.
Case Report
A 44-year-old female P1L1 who is not sterilized presented with complaints of excessive bleeding per vaginum for 12 months. The patient was having apparently normal menstrual cycle before 12 months. Cervix and vagina were healthy on per vaginal examination. Pelvic examination revealed a 16-18 weeks sized uterus, firm in consistency. Bilateral fornices were free. No hepatomegaly or splenomegaly. Conventional Papanicolaou test (PAP) smear examination report was mild inflammatory smear with bacterial vaginosis and no evidence of intraepithelial lesion or malignancy. Ultrasonography (USG) revealed presence of calcification (? foreign body) in the anterior fundal wall of Uterus. Other USG findings were Fibroid in posterior wall of uterus and mild hydroureteronephrosis. Hematological investigations were normal. In view of fibroid and completed family, patient underwent total abdominal hysterectomy. Intra-operatively findings were 18 weeks sized uterus and normal ovaries & fallopian tubes. The specimen was sent to pathology department for histopathological examination.
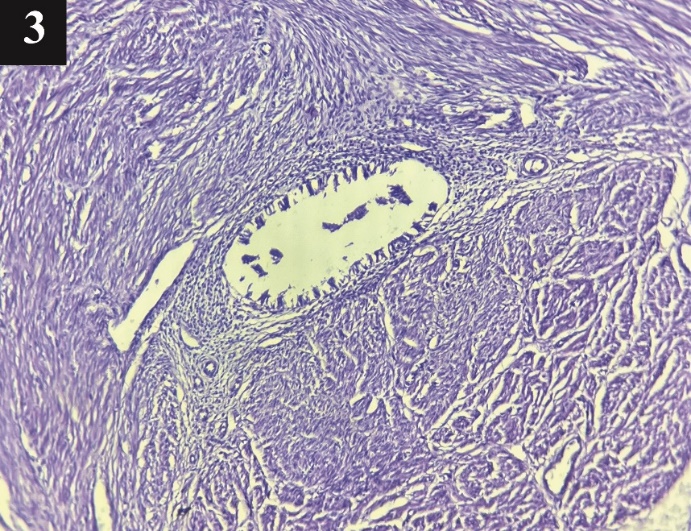
We received Hysterectomy specimen, uterus with cervix measuring 13x11.5x8 cm. Outer surface of cervix was unremarkable. Cut surface of cervix showed endocervical canal measuring 1cm in length. On sectioning uterus, a small bony spicule measuring 1.5x0.4 cm was seen freely lying within the endometrial cavity (Figure 1 A). Endometrial canal was obliterated by trabeculated myometrium (Figure 1 B) with an average myometrial thickness of 3 cm. Endometrial thickness was 0.3 cm. Bits from cervix, endomyometrium and myometrium were given for histopathological examination. The bony spicule within the endometrial cavity was decalcified and all embedded for histopathology.
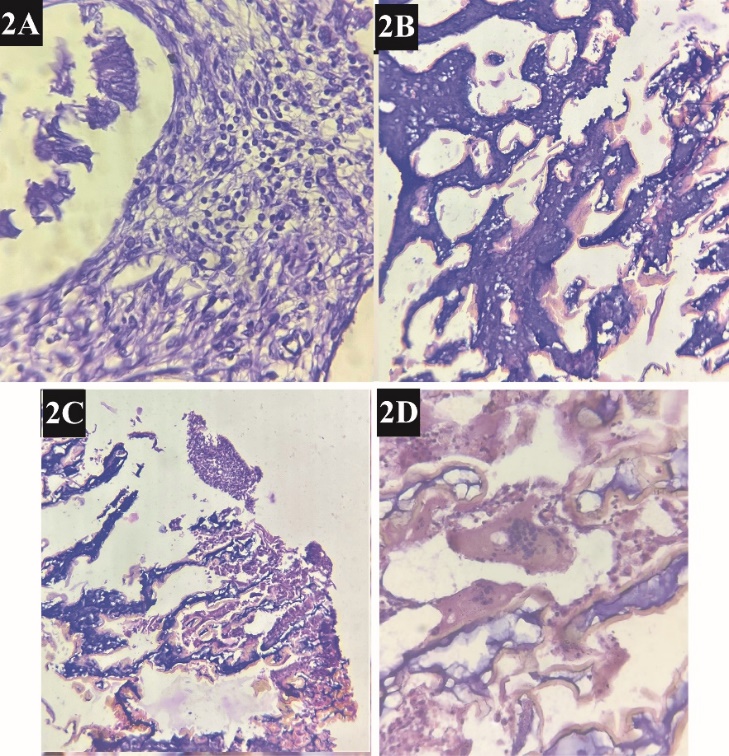
Microscopically, multiple sections studied showed chronic papillary endocervicitis and late proliferative phase endometrium. Endometrial stroma showed chronic inflammatory cell infiltrate composed of lymphocytes and plasma cells suggestive of Endometritis (Figure 2 A). Section studied from bony spicule showed immature lamellar bone with few islands of hematopoietic cells (Figure 2 B-D). Myometrium showed embedded endometrial glands and stroma, suggestive of Adenomyosis (Figure 3). Based on the above findings, retained fetal products can be considered however osseous metaplasia has to be ruled out.
Figure 1
A): Bony spicule that was lying within the endometrial cavity; B): Hysterectomy specimen showing trabeculated myometrium obliterating the endometrial canal
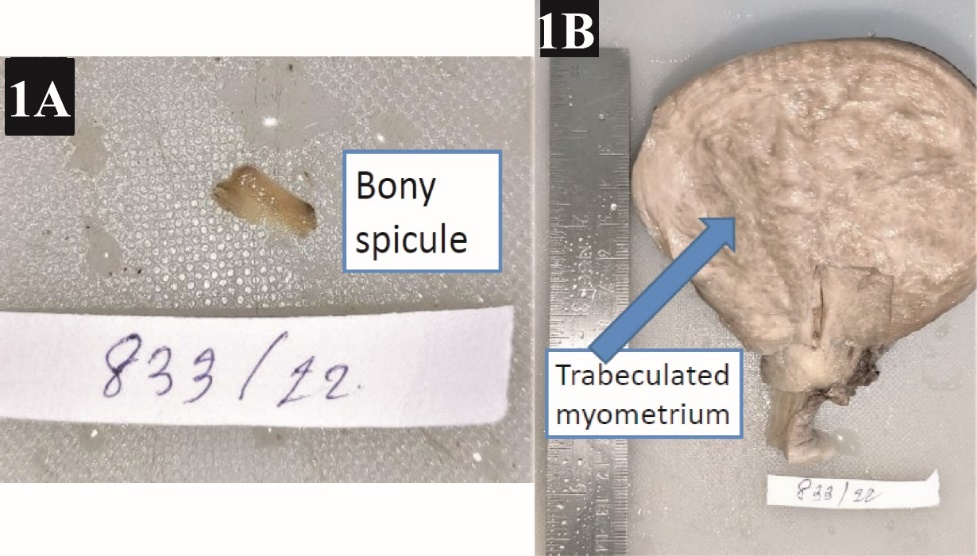
Figure 2
Extramedullary hematopoiesis with underlying endometritis; A): Microphotographic image showing endometrialstroma with chronic inflammatory cells consisting of lymphocytes and plasmacells. 40x H&E stain; B): Microphotographic image showing immature lamellar bone with hematopoietic cells. 10x H&E stain; C): Microphotographic image showing immature lamellar bone with hematopoietic cells. 4x H&E stain; D): Microphotographic image showing immature lamellar bone with osteoclast giant cells. 40x H&E stain
Discussion
Endometrial osseous material within the endometrial cavity with extramedullary hematopoiesis is an unusual entity. Its reported incidence is 3 cases per 10000 women population.1 According to Singh P et al., nine case reports are from India and approximately 80 cases in the entire world have been reported.2 Metaplasia is defined as replacement of one mature somatic cell type to another mature somatic cell type either epithelial or mesenchymal.3 The most common metaplasias occurring in endometrium are mucinous metaplasia, ciliated tubal metaplasia, and squamous metaplasia. The major triggering factors are hormonal or irritative stimuli, sometimes mutation.4 The first documentation of osseous metaplasia of endometrial stromal fibroblasts was by Virchow in 1884.5 In majority of cases, the patients have history of first trimester abortion in reproductive age group. Our case belonged to perimenopausal age group. Various hypotheses have been proposed to explain bone formation within the endometrium. History of abortion is the most common association seen. Retained fetal bones may stimulate endochondral ossification or may cause metaplasia of mesenchymal tissue into bone in response to chronic irritation caused by fetal parts or by dystrophic calcification to retained necrotic fetal tissues.6, 7, 8 A few cases that occurs without the history of pregnancy cannot be explained by this theory, which supports the possibility of true heterotopia where endometrial stromal cells especially fibroblasts are converted into osteoblasts resulting in bone formation. An imbalance between superoxide free radical and superoxide dismutase system has also been implicated in pathogenesis.9 Other possible causes that have been researched are abnormal calcium, vitamin-D and phosphorus metabolism like hypercalcemia (metastatic calcification), hyperphosphatemia and hypervitaminosis D.10 In our case, even though history of abortion is not given, a single bony spicule softly embedded or freely attached within the endometrial cavity and presence of endometritis suggest retained fetal products. Lewis et al.11 also documented the presence of inflammation by the increased concentrations of prostaglandins in endometrial osseous metaplasia. According to Gru AA et al.12 eleven cases of uterine extramedullary hematopoiesis have been reported earlier, among which 2% of cases had the presence of megakaryocytes. However, it is rarely associated with underlying serious hematologic disease. In the present case, there was no underlying hematologic disease. Clinically, the patients may present with infertility due to presence of osseous component within the endometrial tissue preventing the implantation of blastocyst.13 However prompt removal of the bony spicules can restore the fertility. Sometimes patients may present with abnormal uterine bleeding or lower abdominal pain due to associated pelvic inflammatory disease. Tuberculosis has to be ruled out which can have the similar findings. Presence of heterotopic tissues within the endometrial tissue microscopically should also be investigated for carcinosarcoma even though it is rare, especially in postmenopausal women. In this case, the clinical history and gross examination ruled out the possibility of carcinosarcoma.
Ultrasound examination may show an incidental finding of osseous metaplasia, as in our case, however in cases of infertility it plays an important role in its primary diagnosis. In USG, it has a characteristic hyperechogenic pattern. First thing to be ruled out is presence of intra-uterine device. In absence of history of intra-uterine devices, hysteroscopy is both diagnostic and therapeutic in patients with osseous metaplasia. In extensive osseous metaplasia where bony spicules are deep within the myometrium, use of laparoscopic control has been reported in prevention of uterine perforation.7 In our case, total abdominal hysterectomy was done in view of provisional diagnosis of fibroid, which is curative for endometrial osseous metaplasia as well.
Conclusion
Endometrial osseous metaplasia/ osseous component even though rare, important considerations to be kept in mind for non-IUD users are retained products of conception, tuberculosis and rarely serious hematologic disease has to be ruled out especially with finding of extramedullary hematopoiesis. The history of abortion being the most common association is not given by the patient in this case, however retained fetal products cannot be ruled out. Clinicopathological correlation starting from clinical history to basic investigations and ancillary tests help to narrow similar differentials and to identify a specific etiology. In case it is associated with serious pathology, early diagnosis after ultrasound screening can help in the better management of these patients.