- Visibility 48 Views
- Downloads 15 Downloads
- DOI 10.18231/j.ijpo.2022.093
-
CrossMark
- Citation
Choroid plexus carcinoma: A case report
Introduction
Choroid plexus tumours (CPT) are rare intraventricular papillary neoplasms arising from choroid plexus epithelium.[1] They constitute 0.77% of all brain tumours. Choroid plexus carcinoma (CPC) is a rare malignant epithelial neoplasm (WHO grade III) accounting for 34% of CPT.[2] A majority of CPCs (80%) occur in children with a predilection for posterior fossa and are associated with a poor prognosis.[2], [3] We report a case of CPC diagnosed in a 11-month-old boy and discuss the clinicopathological features.
Case Report
A 11-month old male child presented with irritability and vomiting. On examination, the child was irritable with delayed developmental milestones. There was bulging of anterior fontanelle and head circumference was increased (50.5 cm).
Contrast enhanced computed tomography (CECT) brain showed a large lobulated irregular hyperdense lesion in body and occipital horn of right lateral ventricle (LV) and extending into adjacent brain parenchyma with mild perilesional edema and hydrocephalus. Magnetic resonance imaging (MRI) brain with contrast revealed a large 7.1×6.6×4.1 cm intraventricular mass lesion with haemorrhagic foci in trigone, occipital horn, body of right LV with extension to the right occipital brain parenchyma and with edema in right parietal region along with moderate to severe hydrocephalus. MRI whole spine with contrast showed leptomeningeal metastasis.
Craniotomy was performed and the excised tissue was sent for cytology and histopathological examination.
Grossly ([Figure 1] A,B) multiple grey-brown soft tissue bits were received altogether measuring 3×2×1cm. Surface showed minute papillary projections and cut surface was grey-white.


Squash cytology ([Figure 2]) revealed highly cellular smears showing pleomorphic cells arranged in irregular papillary pattern and individually scattered with hyperchromatic irregular nuclei along with mitotic figures and necrotic foci.
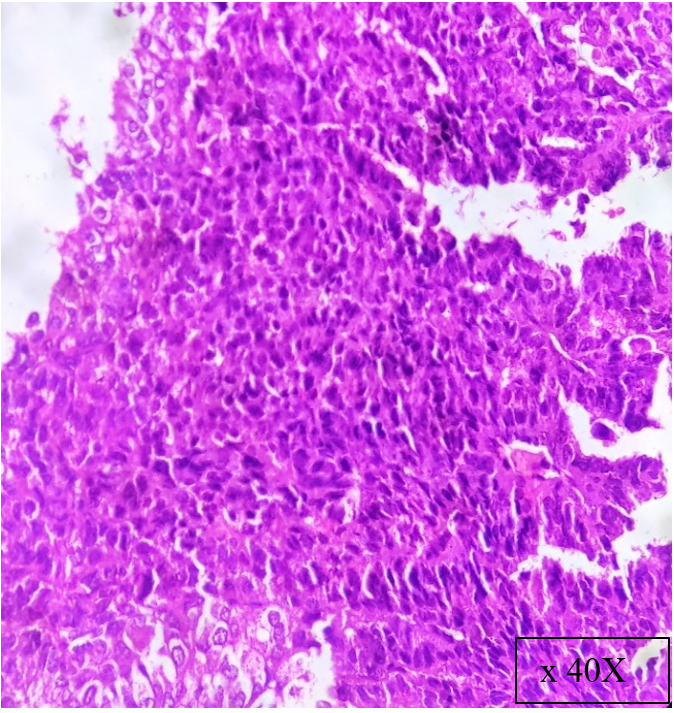
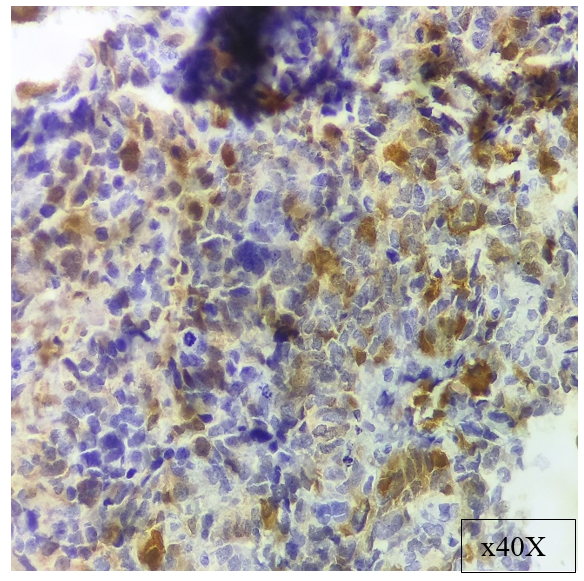
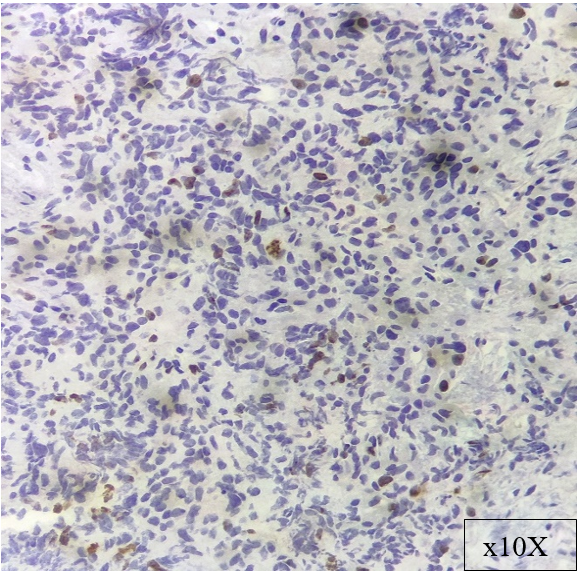
Histopathological examination ([Figure 3]) revealed tumour tissue arranged in papillary pattern with increased cellular density and also in sheets. Neoplastic cells show pleomorphism with irregular hyperchromatic nuclei. There was increased mitotic activity (10-12/10 hpf) with focal areas showing necrosis. Neoplastic cells were immunoreactive for S-100 ([Figure 4]) and Ki-67 proliferation index ([Figure 5]) was 40% in areas of highest proliferative activity. A diagnosis of CPC was rendered.
Discussion
CPC is a WHO grade III epithelial neoplasm arising from choroid plexus epithelium.[1], [2] It mainly occurs in children with a median age of presentation of 3 years.[2], [4] Most cases occur in lateral ventricles followed by fourth ventricle. CPCs can also arise in the cerebellopontine angle, cerebellomedullary cistern, suprasellar cistern, even in sacral canal.[5], [6]
CPCs present with cerebrospinal fluid (CSF) pathway obstruction causing symptoms related to hydrocephalus including headache, nausea, vomiting and enlarged head size.[2], [7] They present as large intraventricular lesions with irregular enhancing margins with edema in adjacent brain, hydrocephalus and disseminated tumour on MRI. Approximately 21% of cases present with metastases at diagnosis.[2]
Grossly CPCs are solid tumours with intratumoural haemorrhage and necrosis often invading adjacent brain.[6] Smears of CPC are hypercellular composed of irregular papillary clusters and single cells with hyperchromatic irregular nuclei, prominent nucleoli with background showing necrosis.[8] Microscopically they show frank malignant histologic features characterized by increased cellular density, nuclear pleomorphism, frequent mitosis, blurring of papillary growth pattern and necrosis. CPCs show immunoreactivity for cytokeratins, less frequently for S-100, transthyretin and is negative for EMA.[2], [6]
CPCs are associated with losses of chromosome 5, 10q, 18q and 22q and gains on 1, 4, 8q, 9p, 12, 14q, 20q and 21.[6] TP53 mutations are seen in 50% cases.[2]
The main differential diagnosis of an intraventricular papillary tumour includes atypical teratoid/rhabdoid (AT/RT) tumours, papillary variant of ependymoma, papillary meningioma and metastatic tumours. AT/RT is composed of groups of rhabdoid cells with eccentric pleomorphic nuclei and abundant eosinophilic cytoplasm with increased mitotic figures and necrosis. CPCs stain positively for INI1 while AT/RT is negative. Papillary variant of ependymoma can be diagnosed by its characteristic histomorphological features, including monomorphic cuboidal cells with indistinct nucleoli, granular chromatin, ependymal rosettes and perivascular pseudorosettes. Papillary meningioma can arise in choroid plexus especially in the paediatric age group. It is characterised histologically as having a pseudopapillary or perivascular pattern constituting most of the tumour. 10% patients show metastases of papillary carcinomas to choroid plexus and their immunoprofiles reflect their primaries of origin.[1], [6]
Surgery is the cornerstone of management and patient survival depends on completeness of resection. Gross total resection (GTR) is the most important factor deciding long-term survival and prognosis. Patients who have undergone GTR have significantly better survival rates than those patients who have undergone subtotal resection.[9] Adjuvant chemotherapy can be used after surgery which causes shrinkage of tumour tissue but experience with this modality is limited. Irradiation following surgery is associated with improved survival but this modality is avoided in young children.[10]
CPCs are associated with a poor prognosis. The five-year survival rates are 40-50%. GTR is difficult in all cases because of the tumour’s propensity to invade the adjacent brain parenchyma and metastases through CSF pathways. CPCs with TP53 mutations have significantly lower survival rate.[6]
Conclusion
Choroid plexus carcinomas are rare aggressive epithelial neoplasms arising from choroid plexus most commonly occurring in lateral ventricles of children and associated with a poor prognosis. It should be considered in the differential diagnosis of intraventricular tumours. Gross total resection is the mainstay of treatment. Adjuvant chemotherapy and radiotherapy is provided for older children.
Source of Funding
None.
Conflict of Interest
None.
References
- S Jaiswal, M Vij, A Mehrotra, B Kumar, A Nair, AK Jaiswal. Choroid plexus tumors: A clinico-pathological and neuro-radiological study of 23 cases. Asian J Neurosurg 2013. [Google Scholar]
- D Louis, O Wiestler, W Cavenee, H Ohgaki. . WHO classification of tumours of the central nervous system 2016. [Google Scholar]
- A Singh, S Vermani, S Shruti. Choroid plexus carcinoma: Report of two cases. Indian J Pathol Microbiol 2009. [Google Scholar]
- A Mishra, C Srivastava, SK Singh, A Chandra, BK Ojha. Choroid plexus carcinoma: A case report and literature review. J Pediatr Neurosci 2017. [Google Scholar]
- P Gopal, JR Parker, R Debski, JC Parker. Choroid Plexus Carcinoma . Arch Pathol Lab Med 2008. [Google Scholar]
- J Greenfield, S Love, H Budka, J Ironside, A Perry. . Greenfield's neuropathology 2015. [Google Scholar]
- T Kim, MR Park, EK Hong, HS Gwak. Choroid Plexus Carcinoma in Adults: Two Case Reports. Brain Tumor Res Treat 2019. [Google Scholar]
- C Lacruz, JS DeSantamaría, R Bardales. . Central nervous system intraoperative cytopathology 2014. [Google Scholar]
- P Jameel, A Varma, P Kumari, K Vagha, J Vagha, S Damke. Choroid plexus carcinoma in an adolescent male: a case report. Journal of Medical Case Reports 2021. [Google Scholar]
- J Wolff, M Sajedi, R Brant, M Coppes, R Egeler. Choroid plexus tumours. Br J Cancer 2002. [Google Scholar]
