Introduction
Anywhere on the body, an epidermoid cyst is a benign soft tissue neoplasm that typically affects the phalanges of the fingers or the cranium and manifests as a lytic lesion or a pseudotumor. Males are more likely to be affected than females.1
Manual labourers frequently develop intraosseous epidermoid inclusion cysts, which are typically caused by prior trauma.2
Nodular, fluctuant, subcutaneous lesions that are limited to a single anatomical location are called epidermoid cysts. There might or might not be a connection to inflammation. Soft tissue tumours are uncommon in the head and neck region (7%). Only 1.6% are found inside the mouth.3
It is recognised as an iatrogenic or traumatic lesion, and it might be misleading from a clinical and radiological standpoint.4
Epidermoid bone cysts are well-defined, rounded osteolytic lesions on radiographic examination. According to histopathology, these lesions have a squamous epithelial inner lining with a granular layer that is covered by sheets of laminated keratin that fill the whole cavity. Depending on the clinical presentation, the treatment choices are either curettage or excision.2
It is challenging to make the right diagnosis prior to surgery due to the disease's rarity. In the distal phalanx of the right middle finger, an epidermoid cyst is a rare condition that is described in this paper. We examine the pathologic, radiological, and clinical characteristics of this unusual intraosseous digital lesion. Conservative surgical removal is the recommended course of action for this cyst, and recurrence is rare.
Case Report
A 45-year-old man with a 5-month history of expansion of the distal phalanx of the right middle finger visited us in May 2022. He had no other major medical history. The patient's finger had been injured five months prior to presentation, and the finger had grown gently and painlessly for the first few months. There was no loss of feeling, stiffness, fever, or pain at night. No fractures or other bone lesions were seen at that time. Upon clinical examination, the right middle finger's distal phalanx was enlarged and the nail bed was protruding. Every blood test came back normal. An X-ray of the hand was taken, and the distal phalanx showed a spherical radiolucent lesion with a "ground glass" look.
An expansile hypodense lytic lesion that caused bone expansion and cortical thinning was discovered through radiological analysis. (Figure 1)
Figure 1
Anteroposterior (b) and lateral (a) preoperative radiographs demonstrating a hypodense expansile lesion with cortical thinning

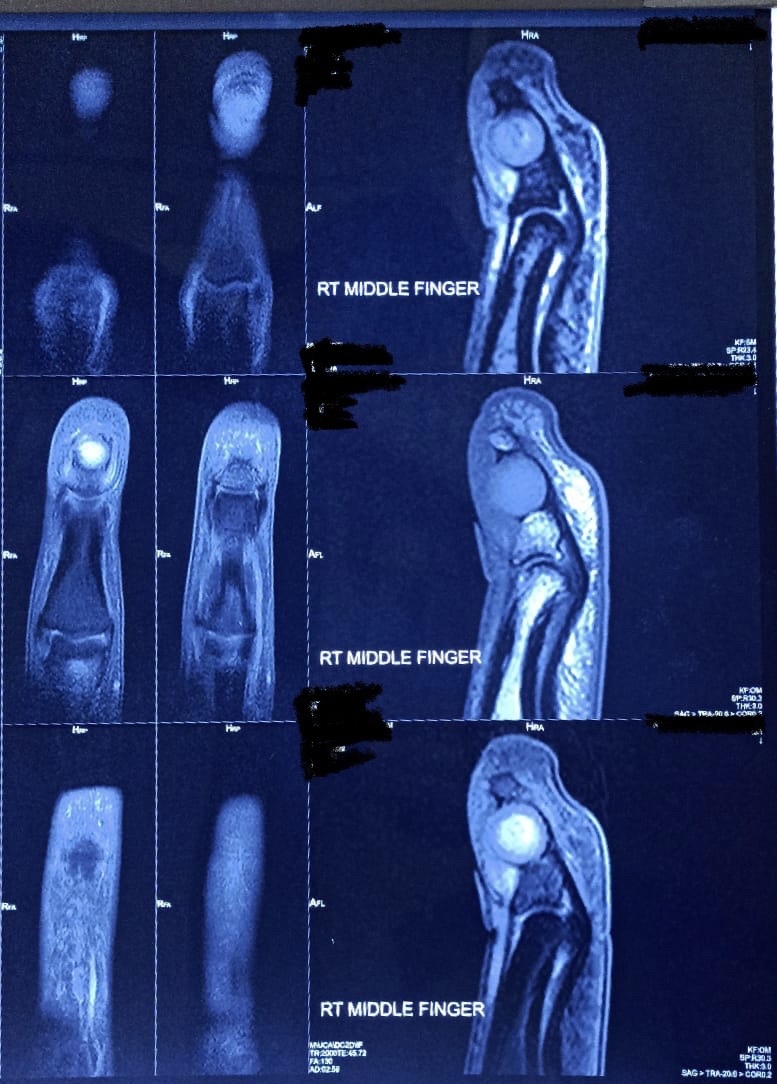
A well-defined spherical lesion measuring 7x7mm was discovered on an MRI of the middle finger's distal aspect. This lesion had eccentric phalanx erosion and was most likely a giant cell tumour or epidermoid inclusion cyst (EIC).(Figure 2)
Figure 2
Preoperative well-defined spherical lesion on the middle finger's distal phalanx with eccentric phalanx erosion
Aspiration Using Fine Needles as suggested by an epidermoid cyst, the lesion's cytology revealed mature squamous cells against a background of necrotic material and amorphous keratin.(Figure 3)
Figure 3
a,b,c,d: Mature squamous cells can be seen in cytology smears against a background of necrotic material and amorphous keratin

At the time of surgery, the lesion site had a thinning bone cortex that looked like an eggshell and contained a thick, creamy substance in addition to a thick layer of tissue from the lesion's interior chamber.
The specimen was a single, delicate, grey-white bit of tissue that was 1.5 x 1.0 x 0.5 cm in size.(Figure 4)
The wall of the cyst was made up of stratified keratinizing hyperplastic squamous epithelium, according to histopathology examination. The subepithelial tissue supported the suggestive diagnosis of an epidermoid inclusion cyst by containing fibro collagenous stroma, mild chronic inflammation, and many thin walled blood vessels.(Figure 5, Figure 6)
Figure 5
According to histopathology, the cyst wall is made up of stratified squamous epithelium that is hyperplastic. The subepithelial tissue exhibits fibro collagenous stroma, mild chronic inflammation, and many blood vessels with thin walls

Figure 6
According to histopathology, the cyst wall is made up of stratified squamous epithelium that is hyperplastic. The subepithelial tissue exhibits fibro collagenous stroma, mild chronic inflammation, and many blood vessels with thin walls

The patient's postoperative recovery went smoothly.
Discussion
Rare bone cysts called epidermoid bone cysts typically affect the skull and phalanges. The distal phalanx of the fingers is where phalangeal involvement most frequently occurs.1, 4, 5
The majority of intraosseous epidermoid cysts are single lesions, although in a small number of cases, patients have complained of cysts affecting several fingers on the same hand. These lesions are thought to have developed as a result of trauma and were brought on by the invasion of epidermal tissue into the bone.3
The aetiology of intraosseous epidermal inclusion cysts remains unknown. While a congenital aetiology with intraosseous inclusion of embryonal epithelial tissue has been proposed, a post-traumatic origin remains the most prevalent hypothesis as many patients do recall an antecedent traumatic event or surgical procedure in the identified lesion.6 It may be the result of major or minor digital trauma to the terminal phalanx which may have occurred many years prior to the presentation.7 A remote or recent history of digital trauma should be sought to narrow the diagnostic possibilities. Symptoms may present at a variable amount of time (i.e., months to years) following the inciting event.6
Some studies have suggested that the origin of a phalangeal cyst is either directly caused by traumatic implantation of epidermal fragments into the bone by any type of injury, or due to migration of a fragment of the nail bed into the phalangeal bone.8
It is surmised that superficial epithelial cells are displaced into the underlying osseous compartment following digital trauma or surgery.6 Clinicians claim that traumatic implantation of cystic cells into deeper tissues with subsequent cystic change and expansion is the major etiological factor for formation of intraosseous epidermoid cysts.3
Careful clinical examination and radiographic examinations are the initial steps in making the right diagnosis. The intraosseous epidermoid cyst typically presents radiologically as a well-circumscribed, growing radiolucent bone lesion with frequently evident soft tissue oedema. Despite its limited ability to define bone abnormalities, MRI is beneficial in identifying secondary injuries and determining how invasive the injury is to the surrounding tissue.2
Epidermoid bone cysts can be difficult to diagnose clinically and radiologically. A chondroma, intraosseous ganglion, bone cyst, giant cell tumour, or even a metastatic lesion are examples of differential diagnoses.8 On a clinical and radiological examination, it is challenging to distinguish between these entities. Making a certain diagnosis is aided by histopathological analysis.7 Radiographically, it is challenging to distinguish from other radiolucent lesions.6 The differential diagnosis of a radiolucent osseous tumour of the finger should take an epidermoid cyst into account.9
In contrast to the pattern of poorly defined osteolysis that accompanies skeletal infection and metastasis, the radiological features seen in phalangeal or cranial bones with epidermoid cysts are well known well defined osteolytic lesions with a sclerotic margin, with or without soft tissue swelling.8 To prevent recurrence, adequate curettage and excision of the cyst capsule are crucial.8 In situations of expansile lytic lesions of the distal phalanx with a history of penetrating or blunt trauma, epidermal inclusion cyst should be taken into consideration as one of the diagnoses.7
If enough keratin or sebaceous material is recovered, a needle aspiration may be adequate for making an accurate preoperative diagnosis; however, in the majority of cases, histopathological investigation is required for the correct diagnosis.10 Intra-lesional curettage, with or without bone graft, is the surgical procedure used to treat EIC. It is possible to anticipate an uneventful recovery with no signs of recurrence during short-term follow-up. According to the scant published literature, no cases of recurrence after curettage have been documented.6 Conservative surgical removal is the recommended course of treatment for epidermoid cysts.3
Conclusion
In conclusion, intraosseous epidermoid inclusion cysts are uncommon clinical conditions with a history of trauma. The differential diagnosis should take benign or malignant radiolucent osseous neoplasms into consideration. The importance of having a high index of suspicion regarding radiolucent bone lesions of the distal phalanx, especially in patients who have experienced prior trauma, was highlighted by this case report for both clinicians and pathologists. Additionally, the diagnosis of intraosseous epidermoid cyst should always be taken into consideration.

