Introduction
Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome is a type of idiosyncratic drug reaction causing systemic symptoms, morbidity and mortality. Common precipitating drugs are antiepileptic drugs, anti-tubercular drugs (ATD), antibiotics, and anti-inflammatory drugs.1, 2, 3, 4 We report a case of DRESS syndrome, diagnosed based on clinical history, examination findings and laboratory investigations.
Case Report
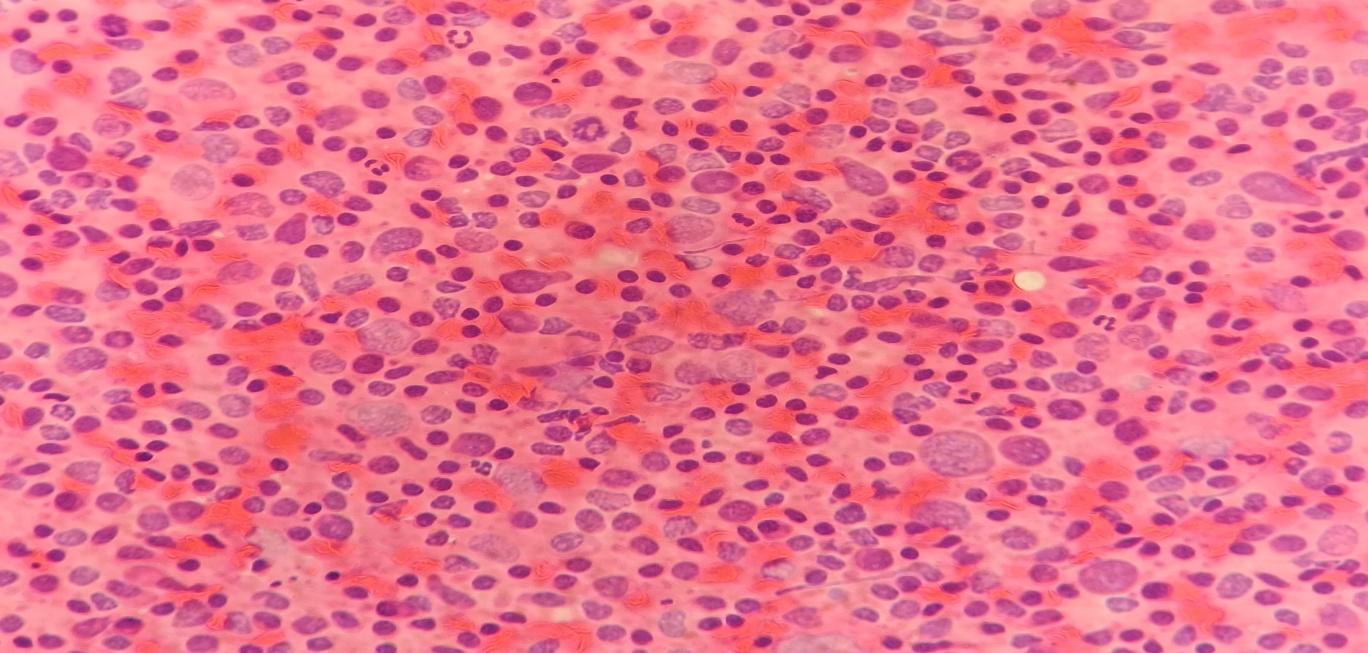
50 years old male came with tuberculosis on short regimen of multidrug drug resistant (MDR) pulmonary tuberculosis for the last one month. He had complaints of generalized erythema, puffiness and itching of the whole body for 2 days. The erythematous lesion started as maculopapular rash, slowly desquamated and became exfoliative. Bilateral inguinal lymphadenopathy was noted with right side being larger (3X2 cm). Total leukocyte count was increased (neutrophils 40.1%, lymphocytes 26.8%, monocytes 12.5%, eosinophils 17.5% and basophils 3.2%). Bilirubin, SGOT, SGPT and ALP were raised. Viral markers were negative. FNAC from the inguinal lymph node showed a polymorphous population of lymphoid cells with few revealing mild nuclear enlargement and opened up chromatin. No definite Reed- Sternberg cells, indented/ irregular nuclei or granulomas were identified (Figure 1). Symptoms were drastically improved with withdrawal of ATD and treatment with corticosteroids and antihistamines. Score of 6 was obtained as per British Association of Dermatologists (BAD) DRESS scoring system.5 Thus definite diagnosis of DRESS syndrome was given.
Discussion
The term DRESS syndrome was coined by Bocquet et al for the severe adverse drug reactions develops after a latency period.3 Common precipitating drugs are anticonvulsants, antimicrobials, antitubercular, antiviral, anti-inflammatory and herbal medicines.1, 2, 3, 4 The symptoms usually develop after three weeks of exposure to offending drug.
Theories suggested for etiology are genetic deficiency of metabolic enzymes leading to accumulation of toxic metabolites, genetic predisposition among individual with specific HLA haplotype, reactivation of viruses (Epstein Barr viruses/ herpetic viruses) and immunological mechanisms related to elevated levels of inflammatory cytokines.1, 2, 3
Patients present with history of drug intake, fever and skin manifestations like rash involving > 50% of total body surface area (can even develop into erythroderma). They are macular, papular, maculopapular, exfoliative or pustular lesions. Facial edema is also common. Skin biopsy shows spongiosis, dense perivascular lymphocytic infiltrate in papillary dermis along with eosinophils and atypical lymphocytes.2, 4
Hematological manifestations include leukocytosis with eosinophilia, lymphocytosis, lymphocytopenia, atypical lymphocytosis and thrombocytopenia. DRESS syndrome also affects internal organs like liver (elevated hepatic enzymes), kidney (interstitial nephritis and acute tubular necrosis), lungs (deranged pulmonary function tests, interstitial pneumonia and acute respiratory distress syndrome), heart (hypersensitivity myocarditis and acute necrotizing eosinophilic myocarditis), gastrointestinal tract, pancreas, spleen and nervous system (headache, seizure and motor neuron involvement).1, 2, 4
Localized or generalized lymphadenopathy is common (75% of cases).2 FNAC shows polymorphic population of large immature and mature lymphoid cells, histiocytes and macrophages. Lymphomatous and non-lymphomatous causes are considered in such cases. Presence of numerous neutrophils (Acute lympahadenitis), plasma cells (Rheumatoid arthritis), eosinophils (Kimura disease) and emperipolesis of inflammatory cells (Rosai –Dorfman disease) needs to be ruled out. Multinucleated giant cells (granulomatous conditions, infectious mononucleosis) granulomas, necrosis (necrotizing granulomas and Systemic lupus erythematosis), karryorrhectic debris (Kikuchi disease) and prominent capillaries needs further evaluation. Reed-sternberg cells (Hodgkin lymphoma), LE cells (Systemic lupus erythematosis) and indented/ irregular nuclei (Langerhans histiocytosis/angioimmunoblastic T cell lymphoma) are absent.
Diagnosis of DRESS syndrome by Bocquet et al. needs all the three features like skin eruptions, eosinophilia/ presence of atypical cells and involvement of internal organs.3 The RegiSCAR group proposed a criteria for hospitalized patients with rash to diagnose DRESS syndrome. According to Japanese group’s criteria, the presence of seven features are needed for diagnosis [maculopapular rash developing >3 weeks after starting with the suspected drug, prolonged clinical symptoms 2 weeks after discontinuation of the suspected drug, fever, liver abnormalities, leukocyte abnormalities, leukocytosis, atypical lymphocytosis (>5%), eosinophilia, lymphadenopathy and Human Herpes 6 reactivation].3
Scoring system by BAD classifies patients based on presence of fever, eosinophilia, enlarged lymph nodes, atypical lymphocytes, rash, organ involvement, disease duration and skin biopsy/investigations expressing alternate causes. The score ranged from -2 to 2. Total score <2 excludes and score of 2-3, 4-5 and ≥6 classified as possible, probable and definite diagnosis of DRESS syndrome.5
Rifampicin is the common ATD associated with this. Isoniazid, Ethambutol, Pyrazinamide, Fluroquinolones, Para-amino Salicylic acid, Streptomycin can also cause this syndrome.5, 6
Because of combination therapy, detection of the culprit drug is difficult. In the study by Allouchery et al, 67 among 2154 adverse drug reactions to ATDs were diagnosed with DRESS syndrome. (60 were associated with Rifampicin and 32 with Isoniazid). Though Rifampicin is the most common ATD associated with DRESS syndrome, among tuberculosis cases Isoniazid is found to be the most suspected drug (due to non-tubercular uses of Rifampicin). After extensive search we have not come across any literature mentioning the percentage of multidrug resistant ATD associated with DRESS syndrome among all ATD associated with DRESS syndrome. ATD associated DRESS syndrome usually occurs at recommended doses of these drugs (no dose dependent effect).5 In our patient the DRESS syndrome could have occurred with Isoniazid or any of the multidrug resistant ATD. It is important to recognize the presence of DRESS syndrome in MDR tuberculosis patients who already had this syndrome.
Precipitating drugs (detected by skin patch and lymphocyte transformation tests) are contraindicated, however due to the absence of alternative drugs and nature of the infection, reintroduction of these drugs can be offered based on the risk/benefit ratio.6
Treatment includes immediate stoppage of offending drugs followed by steroids and other supportive measures. Mortality rate is around 10%.2 (due to long-lasting internal organ damage and reactivation/secondary infection to steroid therapy). Clinical differential diagnoses are Steven jonhson syndrome/ toxic epidermonecrolysis, hypereosinophilic syndrome and Kawasaki diseases.2
Conclusion
DRESS syndrome is life threatening condition which needs timely diagnosis and management for saving lives.1, 2 ATDs are common drugs causing this. Though there are no definite diagnostic traits for DRESS syndrome, in lymph node FNAC, we need to search for features to rule out other etiologies. Our case highlights the importance of cytology in diagnosis of DRESS syndrome.