Introduction
A bunch of mysterious pneumonia cases was reported by the Chinese population to the World Health Organization (WHO) on 31 December, 2019.1 The etiology for this outbreak was a novel corona virus named severe acute respiratory syndrome corona virus 2 (SARS-CoV-2), which was responsible for the Corona Virus Disease 2019 (COVID-19).2 And by January 2020 the disease became epidemic and was observed internationally, cases have been reported in 24 countries and 5continents.3
Although it is well expected that COVID-19 is primarily manifested as a respiratory tract infection, up-and-coming data indicate that it should be regarded as a systemic disease involving multiple systems, including cardiovascular, respiratory, gastrointestinal, neurological and hematopoietic and immune system.4 Patient’s clinical manifestations included fever, nonproductive cough, dyspnea, myalgia, fatigue and radiological substantiation of pneumonia. Organ dysfunction (e.g., shock, acute respiratory distress syndrome [ARDS], acute cardiac injury, and acute kidney injury) and death can occur in severe cases.1 Early diagnosis is vital when bearing in mind the short time of onset of acute respiratory distress syndrome among patients after admission to hospital and the high mortality rates in COVID-19.
Blood tests have an important role in early diagnosis of the disease, considering the information they provide to physicians regarding the inflammatory process. Complete blood counts (CBC) are easily performed and cheap. Included in the CBC are values such as white blood count, neutrophil, lymphocyte and platelet count (PLTs). These parameters may be used as inflammatory markers by themselves, their ratios to one another may also be indicators of early inflammation.1 Considering previous research, the use of circulating biomarkers in lieu of inflammation and the immune system have been considered as a prognostic indicator in COVID-19-positive patients.
In this study, the roles of biomarkers from a peripheral blood sample is used in the diagnosis of COVID-19 patients who have history of fever and have been admitted to hospital are examined.
Materials and Methods
A retrospective study was carried out in a private sector hospital at Panipat where the patients having history of fever were admitted during 1st May 2020 to 15th August 2020. A total of 100 patients were included who were suspected cases of corona. RTPCR was done for all the patients and were categorized into covid negative and covid positive patients.
All the blood parameters, Systemic inflammatory index (SII) = thrombocyte count × neutrophil count/lymphocyte count. Neutrophil lymphocyte ratio (NLR) = absolute neutrophil count/absolute lymphocyte count. Platelet lymphocyte ratio = absolute platelet/absolute lymphocyte count were calculated. Coagulation factor (prothrombin time(PT), activated partial thromboplastin time (aPTT), international normalized ratio(INR) and C-Reactive protein (CRP) were compared between negative and positive COVID-19 cases.
The analysis of the data was done using the SPSS 25 statistical package programs. A Chi-square test was used to analyze the resounding variables of the patients, which were expressed as a number and percentage. The independent samples t-test was used for analysis for parametric continued variables and they were presented as a mean as well as standard deviation. The Binary Logistic Regression test was used to assess the diagnostic utility of several biomarkers to define risk ratios, including the SII. A receiver-operating characteristic (ROC) curve was formed, the Youden’s index (J) used for cut-off values in the diagnosis of COVID-19 and the area under the curve (AUC) was calculated, p < 0.05 was considered statistically significant.1
Results
Out of 100 patients included in the study that came with history of fever and was admitted in hospital, RTPCR was done and 65% patients were positive. Out of which 66.2% were male patients and 33.8% were female patients as shown in Figure 1. The mean age of positive patients was 43.03years with standard deviation of 16.1.
Hematological parameters were recorded and presented in a tabular data as described in Table 1. Parameters included were total leukocyte count, neutrophils, hemoglobin, lymphocytes, NLR, PLR, SII, and Platelets. In patient with negative test results, it was found that total leukocyte count, neutrophils, platelet, NLR and SII values were higher. Whereas haemoglobin, lymphocytes and PLR was found to be higher in patients with positive test results.
Table 1
Comparison of haematological parameters according to RTPCR test results
Since there was a statistically significant disparity between negative and positive groups according to parameters (leukocyte, neutrophil hemoglobin, platelet, NLR, PLR and SII), they were then studied with ROC analyses. Regarding the observations made by ROC analyses, the following information concerning patients with COVID-19 diagnoses were found (Table 1 & Figure 2). As shown in Figure 2 hemoglobin, lymphocyte and PLR was noted towards the positive side of the curve.
Figure 1
Receiver operating characteristic curve for significant markers in the prediction of corona virus positive patients
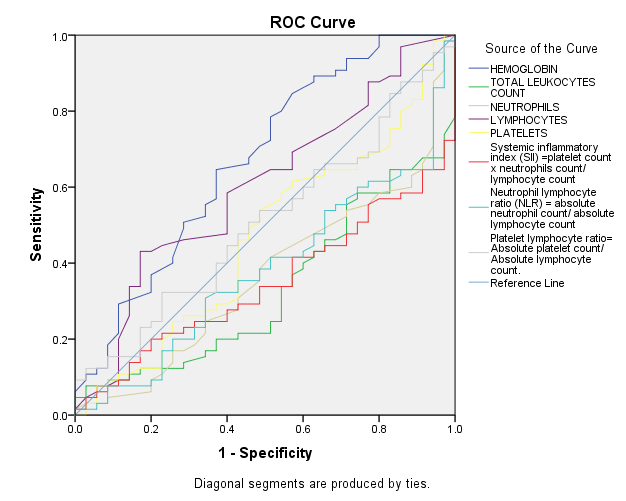
TLC, Neutrophils, platelets, SII and NLR could not be used as a potential diagnostic biomarker for subsequent analysis because its AUC was less than 0.50. The optimal cut-off values were 11.25, 22.5 and 201.8 for hemoglobin, lymphocytes and PLR.
Table 2
Area under the curve for hemoglobin, TLC, Neutrophils, lymphocytes, platelets, SII, NLR and PLR
The optimal cut-off values were 11.25, 22.5 and 201.8 for hemoglobin, lymphocytes and PLR. Comparisons were made between these two groups that were formed according to the cut-off values and correlation was established with PLR where p value was <0.05.
Table 3
Comparision of results according to cut-off points
Further coagulation profile (PT, APTT, INR) and CRP was compared between negative and positive group. P value was assessed and there was strong correlation noted with CRP as shown in Table 4.
Discussion
Taking into account that COVID 19 is highly infective and has high mortality rates early diagnosis of the disease is essential. The authoritative diagnosis of this disease is made by a viral presence in real-time PCR analyses. Due to factors such as the high number of samples, limited number of staff trained in performing the aforementioned tests insufficient lab capacities, the time it takes to receive results can be prolonged. Therefore, every parameter allowing for early diagnosis is vital. Therefore, in this study, the possibility of diagnosing COVID-19 early by a simple, inexpensive, easily accessible test, such as a CBC, has been examined.
Patients who came with history of fever and were admitted in the hospital, RTPCR was performed during the arrival and was found that 65% patients were covid positive and 35% patients were negative out of 100 patients examined.
Table 5
Comparison between current study and other study
In our study COVID 19 positive patients presented with leucopoenia, neutropenia, thrombocytopenia, lymphocytosis, SII and NLR were reduced, PLR and CRP was Increased. PT and APTT were within normal limits. Lymphocyte count and PLR showed strong significance in this study. Comparison was made between current study and various other studies as described in Table 5 where concordance and discordance was seen between different studies.
An obvious relationship, although not definitely proven, exists between a bacterial infection and neutrophilia, and a viral infection and lymphocytosis. Accordingly, NLR of peripheral blood has been used to distinguish between these types of infections. In few studies NLR is higher in those with fever due to bacterial infections than those with fever due to a viral etiology1 however in our study NLR was reduced in COVID-19 positive cases. SII has been proposed as a prognostic indicator in the follow-up of sepsis patients.5 In this study, SII was found to be significantly low for COVID-19-positive patients, meaning that it can also be used while diagnosing COVID-19.
Conclusion
The definitive diagnosis of COVID-19 was made by RT-PCR analysis, but this is a time-consuming and less accessible test. In our study, low values of leukocytes, neutrophils, platelets and high values of hemoglobin, Lymphocytes were found with a CBC test which is easily available are found to be valuable in terms of the initial diagnosis of COVID 19. In addition, low values of NLR and SII and high value of PLR and CRP are also indicative of COVID-19.

