Introduction
Secretory breast carcinoma (SBC) was first described by Mc Divitt and Stewart.1 It is a very rare subtype of breast cancer and constitutes for 0.5% of all invasive breast cancers.2 Originally described as a juvenile breast carcinoma as due to it’s predominance in younger age, it has an indolent behaviour. It is identified by its distinct histomorphology, triple negative immunophenotype and favourable prognosis. We report a case of this invasive carcinoma with secretory morphology exhibiting weak ER positivity and only one basal marker expression.
Case Report
A 46-year-old female patient presented with mass in the left breast since one month. General, systemic examination and routine laboratory investigations were carried out. Local examination showed a mass measuring 5x6cms. Mammography showed the presence of a large, ill defined, lobulated heteroechoic lesion in the retroareolar region of left breast, with significant internal vascularity, suggestive of BIRADS VI. Also noted were multiple small satellite lesions with no internal vascularity, largest at 9 o’clock measuring 2.2 x 1.6cm.
Fine needle aspiration (FNA) performed with a 22-gauge needle, yielded thick material. Highly cellular smears showed numerous papillaroid fragments and dyscohesive clusters of epithelial cells, absence of bipolar bare nuclei in a scant mucinous background, prompting a diagnosis suggestive of malignancy. Core needle biopsy was performed and was sent for histopathological (HP) evaluation.
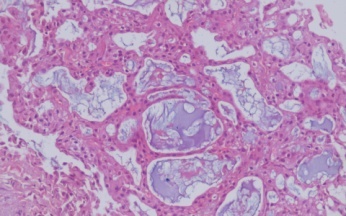
Sections studied showed a neoplasm with tumour cells arranged in microcystic, tubular, focal micropapillary and solid pattern. The tumour cells were large with eosinophilic granular to vacuolated cytoplasm, round to oval hyperchromatic nucleus, with focal conspicous nucleoli. Intracytoplasmic and extracellular eosinophilic to amphophilic secretions were seen (Figure 1, Figure 2). Occasional mitotic figures (4-5/per 10 hpf) seen with moderate tumour infiltrating lymphocytes. No lymphovascular or perineural invasion identified. With these histopathological features, a diagnosis of invasive breast carcinoma with Secretory morphology was made with grade II morphology. Immunohistochemistry (IHC), IHC4 was performed which showed Allred Score for ER of 2+1=3 (Figure 4), Her 2 neu (Figure 5) and PR was negative and Ki67 was 10% in tumour hotspots (Figure 6). Later, EGFR was found to be positive (Figure 7) & CK5/6 was negative (Figure 8).
Chest X-ray, abdominal ultrasound did not show any evidence of metastatic disease. Following an 8 cycle neoadjuvent therapy, the patient underwent modified radical mastectomy with axillary lymphnode dissection and the specimen was sent for Oncopathology evaluation.
Gross examination showed multifocal tumour, larger measuring 7x4x5cm in upper and inner quadrant of breast; smaller tumour measured 1.2x1x1cm and was located in lower outer quadrant. On microscopic evaluation with routine hematoxylin and eosin (HE) staining, the tumour showed pushing margin with morphology similar to core needle biopsy. Other histological features included signet-ring morphology, numerous microcysts, abundant intra and extracellular (within microcysts) eosinophilic material, which was Periodic acid- Schiff (PAS) and diastase resistant (Figure 3). The nucleus of these tumour cells were of low cytological grade. Mitotic activity was sparse and focal areas of necrosis was noted. No in-situ ductal / lobular carcinoma component was identified. All the resected margins were free of invasive tumour. 17 reactive axillary lymphnodes isolated showed no metastasis. Patient was stable in post operative period.
Figure 1
Photomicrograph: H & E; 10x: Microcysts, abundant intra and extracellular eosinophilic material
Discussion
Secretory breast carcinoma is a rare type of breast carcinomas, reported in both sexes. With a median age of presentation as 25 years (range, 3–87 years). The patients commonly present with a slow growing, unifocal painless, well-circumscribed subareolar mass within the breast. Few authors suggest a size larger than 2 cm as linked to an increased malignant potential.3 SBC has a low-grade clinical course and is associated with a favourable prognosis. Our patient is a 46-year-old women with multifocal tumours and of large size.
There are sparse descriptions of mammographic findings in the literature. Due to the frequent occurrence in young woman, mammography may have a diagnostic limitation.
Grossly, it is circumscribed, firm grey white tumour mass with pushing margins.. Secretory carcinoma, histologically is a special type of breast carcinoma with two main features – abundant PAS positive intracellular and extracellular secretions and a granular eosinophilic cell cytoplasm.4 Tumour cells are typically arranged into papillary, microcystic and glandular structures. On Immunohistochemistry, Secretory carcinoma is usually “triple negative” phenotype or may be weakly ER positive.5 Proliferation index by MIB-1 ranges from 1% to 34%.6 CK5/6 and or EGFR positive has been noted in later literature, thus confirming the basal immunophenotype.7 Our case bears weak ER positivity with positive expression of EGFR confirming the basal immunophenotype. Cytogenetically, SBC has been associated with balanced translocation t (12, 15) with associated ETV6-NTRK3 gene fusion.7
Glycogen-rich clear cell carcinoma (GRCC) was the closest differential in our case. It is characterized by the presence of neoplastic cells with a glycogen-abundant clear cytoplasm (the Periodic Acid Schiff–positive, diastase-sensitive).8 But in our case there was presence of abundant PAS positive, diastase resistant intracellular and extracellular secretions and a granular eosinophilic cell cytoplasm, thus favouring a preferred diagnosis of secretory carcinoma.
Surgical excision is the primary mode of the treatment for SBC with sentinel node examination. Distant metastases are extremely rare.9
Conclusion
Secretory carcinoma is a rare variant of breast carcinoma. SBC bears good prognosis despite its basal type Immunophenotype. The histopathological diagnosis of this tumour is quite challenging, inspite of the specific morphologic pattern. Careful interpretation of cytological features, histomorphology in combination with immunohistochemistry ensures the correct diagnosis.







