Introduction
Urothelial neoplasms are one of the most common malignancies in the world.1, 2, 3 Urothelial neoplasms comprise of non-invasive urothelial neoplasms and infiltrating urothelial carcinomas. The urinary bladder is the most common site for cancer development in the urinary tract.4, 5 The lateral wall of the urinary bladder is the commonest site, followed by posterior wall and trigone. In India, according to the recent reports of the National Cancer Registry Programme, the overall incidence rate of the urinary bladder cancer is 2.25% (per 100,000 annually): 3.67% among males and 0.83% for females.6
Nearly 80% of patients fall between 50 and 80 years of age7 with a male to female ratio of 3:1.8 Its development depends on a combination of genetic and environmental factors.9 Bladder tumors are more common in industrial areas (especially in those associated with petrochemicals), and their incidence is increased with exposure to cigarette smoke and arylamines.9, 10, 11 Painless hematuria is the most common presentation.12
The most common important prognostic markers in clinical use are tumour stage and grade.9, 10 Predicting an accurate prognosis with a single factor is difficult, largely due to significant inter-observer variability in reporting the stage and grade.13, 14 Therefore, role of protein and genetic markers as more reliable prognostic factors need to be studied.15, 16
The HER2/neu oncogene encodes for a tyrosine kinase transmembrane growth factor receptor. HER2/neu protein overexpression, assessed by immunohistochemistry (IHC), is associated with increased tumour grade in urothelial carcinoma. 15
Ki67 is a non-histone nuclear protein that is strictly associated with cell proliferation. Tumour proliferation measured by the Ki‐67 is related to tumour recurrence and stage progression in urothelial carcinoma. 16
This study was undertaken to analyze the clinicopathological spectrum of urinary bladder neoplasms and to evaluate the expression of Her2/neu and Ki-67 in malignant lesions. The study has attempted to correlate the Her2/neu expression with the tumour stage and grade, with a view to offer anti-Her2/neu therapies and to establish the role of Ki-67 and Her2/neu as prognostic markers. 17, 18
Materials and Methods
Study population and tissue specimens
This was an observational, cross-sectional, hospital-based study conducted in the Department of Pathology from January 2018 to May 2019. A total of 40 patients were included in the study, of which 39 cases were diagnosed as urothelial carcinoma. The transurethral resection of bladder tumour (TURBT) and Cystectomy specimens were sent from the Department of Urology. The detailed clinical history of the cases was taken. All specimens were thoroughly examined grossly. The volumes of TURBT specimens were measured. In cystectomy specimens, the location of the tumour, gross appearance and infiltration into surrounding tissue was noted. Representative blocks were obtained after thorough sectioning of the tumour. Sections were prepared and stained with haematoxylin and eosin stain. The TNM classification was used for tumor staging and the 2016 WHO classification for tumor grading.19
Immunohistochemistry
Sections were cut from each paraffin block, mounted on poly-l-lysine coated slides and baked on a hot plate at 70ºC for an hour. Slides were then deparaffinized in xylene followed by absolute ethanol and subsequent rehydration in graded alcohol. The secondary detection kit and primary antibodies were used for the immunohistochemistry procedure. Positive controls were taken for the immunohistochemistry staining.
Antibody used in immunohistochemistry:
Evaluation of Immunohistochemistry staining
Ki-67 nuclear staining was observed in 1000 tumour cells and the percentage of cells positive was calculated. Each slide was given a value composed of the sum of staining intensity and the proportion of the stained cells. Scores ranged from 0 to 3+. Scores of 1+, 2+ and 3+ were considered to be positive for Ki-67 expression.20
Her2/neu membranous staining was evaluated using the Ventana pathway Her2/neu protocol. Scoring was done on a scale of 0 to 3+. Scores of 2+ and 3+ were considered to be Her2/neu positive.20
Correlation between tumour stage, histological grade and immunohistochemical expression of Her2/neu and Ki-67 in the cases were assessed.
Results
Clinical profile
The age of the patients ranged from 25 to 80 years, with a mean age of 55.9 years. [Diagram 1] Male to female ratio was 7:1.
The most common presenting feature was painless hematuria (92%) followed by dysuria (8%). 29 patients diagnosed with urothelial neoplasms had a history of smoking, whereas only 3 patients gave a positive occupational history of working in industries. None of the patients gave a positive family history of urothelial carcinoma. The lesion was located in the lateral wall in 22 patients, followed by the posterior wall in 9 cases, trigone in 6 cases and anterior wall in 3 cases.
Histopathological diagnosis
8 cases were diagnosed as low grade non-invasive urothelial carcinoma, 31 cases as infiltrating urothelial carcinoma and 1 case was diagnosed as papillary urothelial neoplasm of low malignant potential (PUNLMP). No high grade non-invasive urothelial carcinoma was reported during the study period. [Table 1]
Among the infiltrating carcinoma cases, 2 cases showed squamous differentiation [Figure 2, Figure 3], 2 cases had glandular differentiation [Figure 4, Figure 5] and 1 case showed sarcomatoid differentiation. None of the cases had any heterologous elements.
4 of the cystectomy specimens were accompanied by lymph node biopsies. Of the 4, 2 cases showed metastasis to the lymph nodes, while the other 2 cases showed reactive hyperplasia of the lymph nodes.
Expression of Ki-67 and its association with tumour grade
The Ki-67 expression was determined by measurement of the Ki-67 score. Scores of 1+, 2+ and 3+ were considered to be Ki-67 positive cases. 30 out of 31 (97%) infiltrating cases showed positive immunohistochemical Ki-67 expression, while 7 out of 8 (88%) low grade cases showed positive immunohistochemical Ki-67 expression.
There was a significant association between the Ki-67 score and the grade of the tumor (p=0.014). [Table 2] There was increase in the Ki-67 score with increase in the grade of the tumour. In infiltrating urothelial carcinoma cases, a higher Ki-67 score was noted, whereas in the low grade non-invasive cases, a lower score was seen.
Score 1+ was present in 5/10 (50%) of infiltrating urothelial carcinoma cases and 5/10 (50%) of low grade non-invasive urothelial carcinoma cases.
Score 2+ was seen in 9/11 (82%) of infiltrating urothelial carcinoma and 2/11 (18%) low grade non-invasive urothelial carcinoma cases.
Score 3+ was seen in 16/16 (100%) of infiltrating urothelial carcinoma cases. [Figure 4, Figure 5]
Only 1 case each of infiltrating carcinoma and low grade non-invasive urothelial carcinoma was negative for Ki-67 immunostaining.
Expression of Ki-67 and its association with tumour stage
Ki-67 expression was determined by the Ki-67 score. Most of the cases with a stage ≥pT2 had a high Ki-67 score (3+) whereas pTa and pT1 had comparatively lower Ki-67 scores. There was a statistically significant association noted between the tumour stage and Ki-67 score (p=0.02). [Table 3]
Expression of Her2/neu and its association with tumour grade
Moderate-to-strong Her2/neu overexpression (2+ or 3+) was observed in 20.5% of the cases. 8 out of 31 (25.8%) infiltrating carcinoma cases showed positivity to immunohistochemical expression of Her2/neu marker [Figure 6, Figure 7], while none of the low grade cases showed positivity to immunohistochemical expression of Her2/neu marker. There was no significant association between tumour grade and Her2/neu expression (p=0.11). [Table 4]
Expression of Her2/neu and its association with tumour stage
Her2/neu expression was noted in 4 pT1 cases and 4 pT2 cases. No significant association was found between Her2/neu expression with the stage of urothelial carcinoma (p=0.178). [Table 5]
Table 1
Relative proportion of cases based on histopathological diagnosis
Table 2
Association of Ki-67 score with the grade of urothelial carcinoma
Table 3
Association between the tumour stage and Ki-67 score
Table 4
Association of Her2/neu expression with the grade of urothelial carcinoma
Table 5
Association of Her2/neu expression with the stage of urothelial carcinoma
Figure 2
Infiltrating urothelial carcinoma with glandular differentiation (arrow head) with Invasion into muscularis propria; H & E stain; 10x
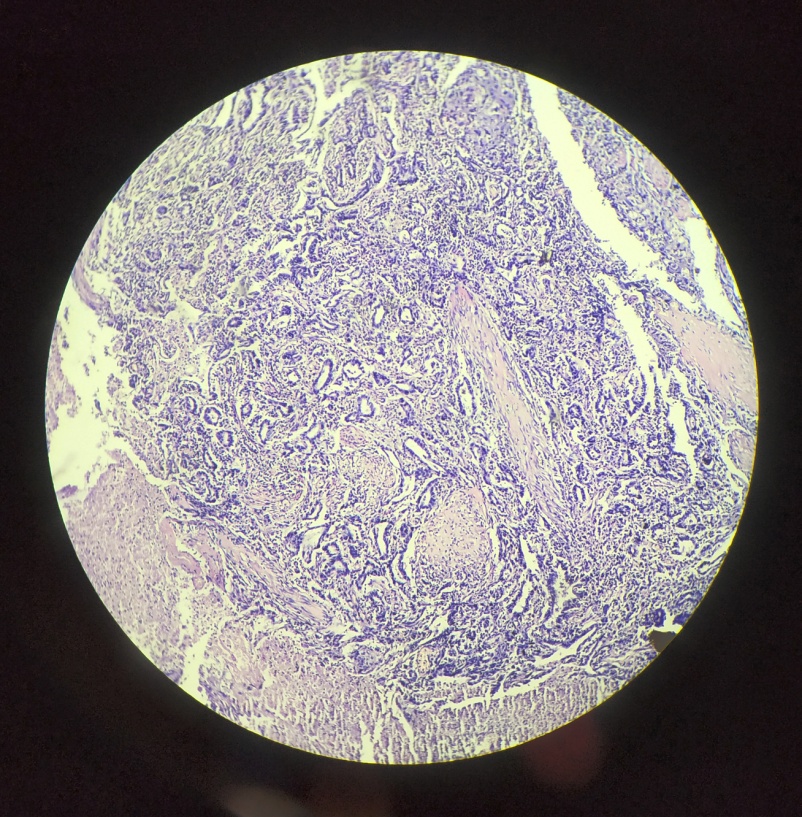
Figure 3
Infiltrating urothelial carcinoma with glandular differentiation (arrow head) with Invasion into muscularis propria; H & E stain; 40x
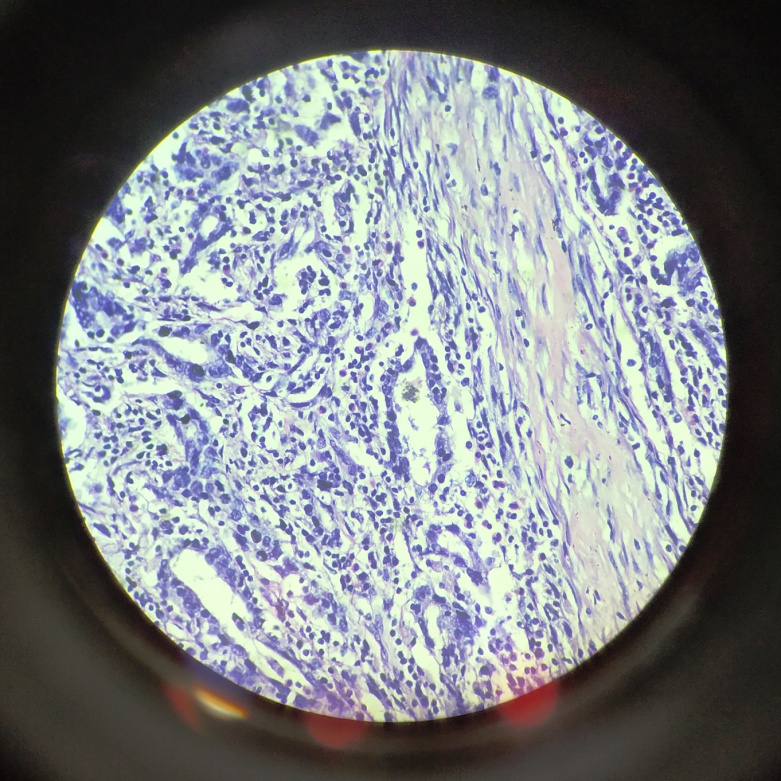
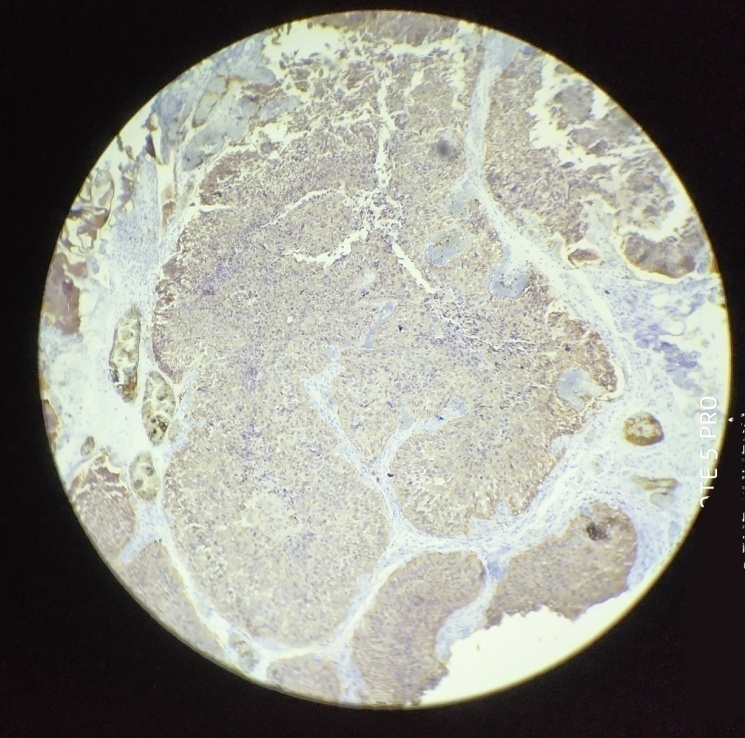
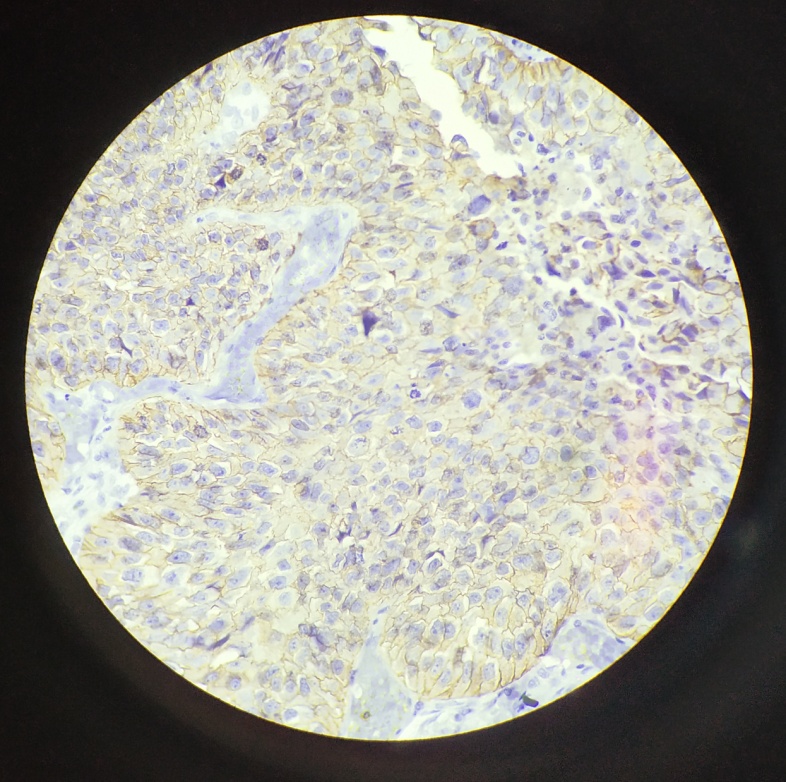
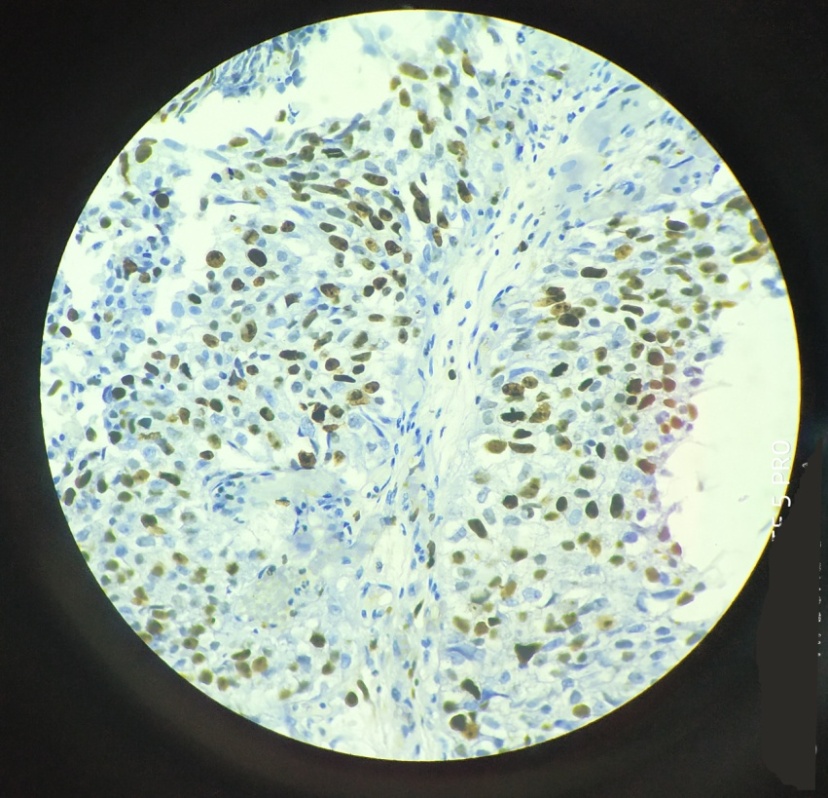
Figure 4
Infiltrating urothelial carcinoma showing score 3+ positive nuclear staining for Ki-67 marker; IHC; 10x
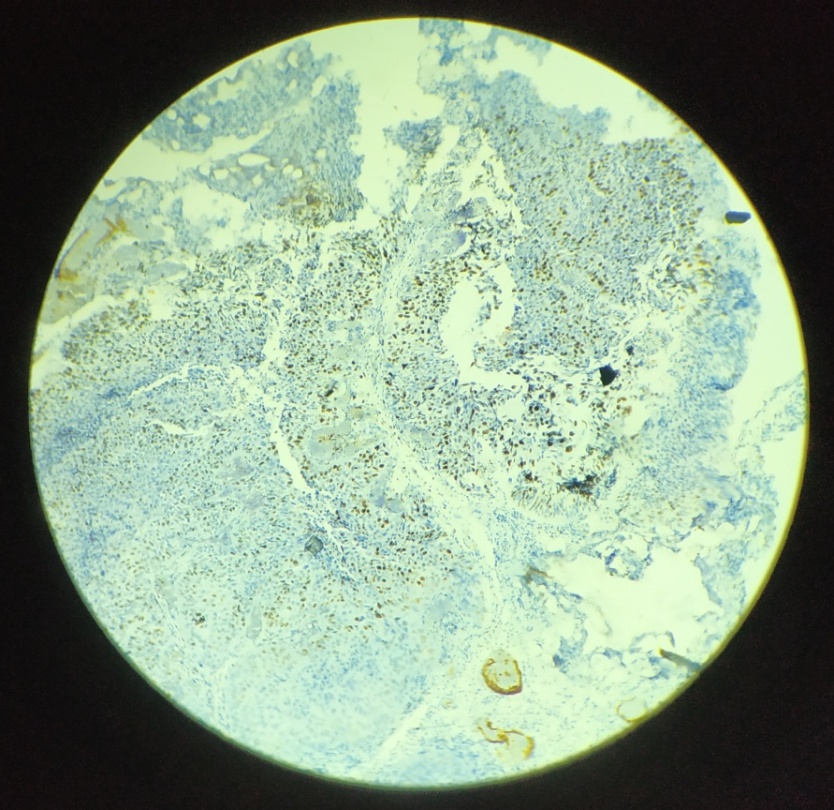
Figure 5
Infiltrating urothelial carcinoma showing score 3+ positive nuclear staining for Ki-67 marker; IHC; 10x (L)
Discussion
The discussion section is organised in the three lines along which our study has progressed: (1) clinical profile of the patients (2) histopathological diagnosis and (3) immunohistochemistry findings.
In this study, the mean age of the patients was 55.9 years, ranging from 25 to 80 years, with a male to female ratio of 7:1. 92% of the patients presented with painless hematuria. These findings were similar to studies by Gupta et al., and Fujii et al.21, 22
Studies by Fortuny et al. and Zeegers et al. have concluded that patients with history of tobacco smoking were at a higher risk of urinary tract cancer.23, 24 In this study, 72% of the patients presenting with urothelial neoplasms had a history of smoking.
8 cases (20%) were diagnosed as low grade non-invasive urothelial carcinoma, 31 cases (78%) as infiltrating urothelial carcinoma and 1 case as papillary urothelial neoplasm of low malignant potential (PUNLMP). No diagnosis of high grade non-invasive urothelial carcinoma was done during the study period. The grading was done in accordance to the updated 2016 WHO classification of urothelial neoplasms.25 It has to be noted that the differentiation of bladder neoplasms may vary from area to area,26 therefore, a biopsy or transurethral resection may show a different grade from the one found in the surgical specimen.27, 28 The grading system has been devised for its application to non-invasive urothelial neoplasms and it does not have much discriminatory power when applied to the invasive component.9, 29 According to Jimenez et al.29 and Cheng et al.,27 histological grade of invasive component provides no additional prognostic information. Infiltrating carcinomas behave as high grade carcinomas.
Staging of the tumours was done according to the AJCC system (American Joint Committee on Cancer). 8 cases were pTa, 18 pT1 and 13 cases were pT2 or higher. It was therefore noted that early stage carcinomas were higher in this study.
96.8% of infiltrating carcinomas and 87.5% of low grade non-invasive carcinomas showed Ki-67 positivity. A similar finding was noted by Jawad et al.30 A significant association between the Ki-67 score and the grade of the tumor was noted (p=0.014), corroborating with the finding of Elkady et al.31
In our study, Ki-67 score was high (3+) in almost all higher stage tumours (≥pT2) and low in the pTa and pT1 tumours. A significant association was noted between Ki-67 score (Ki-67 expression) and the stage of the tumour.
A study by Zambelli et al. observed that Ki-67 scores were significantly related to histological grade and clinical stage.32 Suwa et al. found significant association of Ki-67 expression with both grade and stage of urothelial carcinoma.33 Şentürk et al. found Ki-67 expression in bladder carcinoma increased with pathological stage and histological grade.34
Moderate-to-strong Her2/neu overexpression (2+ or 3+) was observed in only 21% of the cases. This finding was similar to a study by Bellmunt et al. who reported 22% cases as Her2/neu positive.35 Charfi et al. studied 151 cases and reported Her2/neu overexpression in 23% of the cases.36 No statistically significant association was noted between the tumour grade and expression of Her2/neu (p =0.16) in this study. This was similar to a study by Jimenez et al. who did not find the Her2/neu overexpression to be statistically significant.37
No significant association was found between Her2/neu expression and the stage of urothelial carcinoma (p=0.178). This was similar to studies of Alexa et al. who reported a Her2/neu overexpression in 35.59% of the 59 cases studied but found no correlation between HER2/neu overexpression and the tumor stage.38
Conclusion
It was concluded that expression of Ki-67 increased with increase in the grade of the tumour. This finding was suggestive of the prognostic importance of Ki-67. However, there was no significant association between the tumor grade and Her2/neu expression. This study was unable to determine the prognostic value of Her2/neu.
Further studies with a larger population group are required to establish the role of Ki-67 and Her2/neu as prognostic markers.