Introduction
The approach to skin biopsies involves different histomorphological patterns and one such is granuloma formation. The cutaneous granulomatous disorders are seen in both infectious and non-infectious diseases characterized by the presence of granulomas.1 These granulomas develop as a result of an immune system response to an antigen, in which epithelioid macrophages and various inflammatory and immune cells congregate, often surrounded by fibrosis or a lymphocyte cuff.2 Infectious granulomatous dermatoses are more commonly encountered when compared to non-infectious granulomatous dermatoses which are attributed to environmental, socioeconomic and host factors allowing for the easy transmission of pathogens like Mycobacteria leprae, Mycobacterium Tuberculosis and various fungi. Non-infectious granulomatous dermatoses involve a broad group of distinct reactive inflammatory conditions in the skin which are associated with various systemic diseases like sarcoidosis, metastatic Crohn’s disease, methotrexate-induced accelerated rheumatoid nodulosis, xanthogranuloma, granuloma annulare, annular elastolytic giant cell granuloma, necrobiosis lipoidica, interstitial granulomatous drug reaction, foreign body granuloma,etc. These lesions pose a diagnostic challenge to the pathologists because an identical histological picture is produced by several lesions. The present study is undertaken to analyse the morphological patterns of non-infectious granulomatous dermatoses.
Materials and Methods
A retrospective study of skin biopsies was undertaken at the department of pathology in a tertiary care centre of central Karnataka for a period of 5 years from January 2015 to December 2019. All skin biopsies of inflammatory nature obtained by punch or excisional biopsy were fixed with 10% formalin and submitted for processing after gross examination. The sections were stained with routine hematoxylin and eosin (H&E) stain followed by special stains wherever required. Clinical history and relevant data were recorded. All cases were examined in detail and histopathological features of granuloma, location of granuloma, dermal and epidermal changes were noted. Descriptive statistical measures like percentages and proportions were utilized to present the data.
Results
A total of 7273 skin biopsies were received during our study period. Of these, 575(8%) cases were diagnosed as granulomatous dermatoses and 34(6%) cases of them were non-infectious granulomatous dermatoses. The most common diagnosis of non infectous granulomatous lesion was granuloma annulare(50%) followed by annular elastolytic giant cell granuloma(14%), foreign body granuloma(9%), tattoo granuloma (9%), perforating folliculitis(9%), xanthoma (6%) and xanthelasma(3%)(Table 1). Non-infectious granulomatous dermatoses were predominant among females (Table 1).
Table 1
Distribution of non infectious granulomatous lesion
Table 2
Distribution of non-infectious granulomatous lesion among different age group
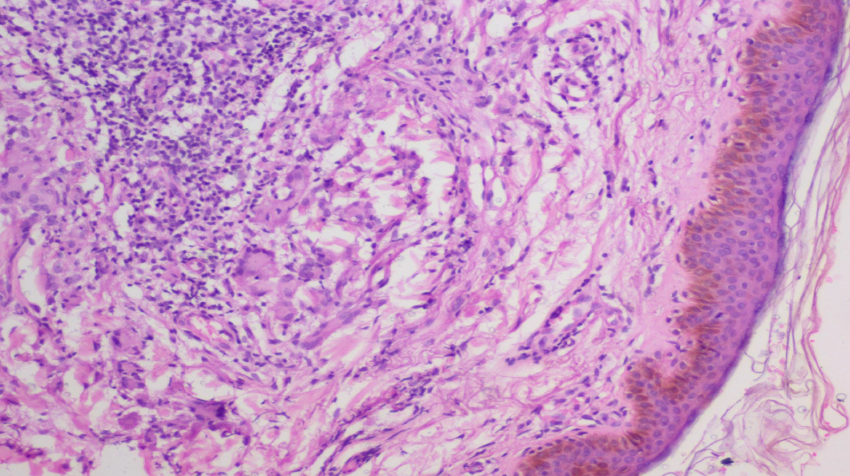
Granuloma annulare was diagnosed in 17 (50%) cases with a female predominance. The most common location was over extremities. Microscopically these cases showed periadnexal lymphohistiocytic infiltrate, palisading of histiocytes with foci of degenerated collagen (necrobiotic areas) and mucin degeneration.(Figure 1, Figure 2)
Two cases(6%) of xanthoma and one case of xanthelasma(3%) were identified in the age group of 31-40 years. Clinically these lesions were located near the eyelids and histologically showed xanthogranulomas comprising of foamy histiocytes admixed with lymphocytes and occasional multinucleate touton type of giant cells. These cases were evaluated for altered lipid profile but all parameters were within normal limits.
Foreign body granulomas were identified in 3(9%) cases with a female predominance. Histologically, these lesions showed granulomas with foreign body multinucleate giant cells admixed with neutrophils and occasional plasma cells.
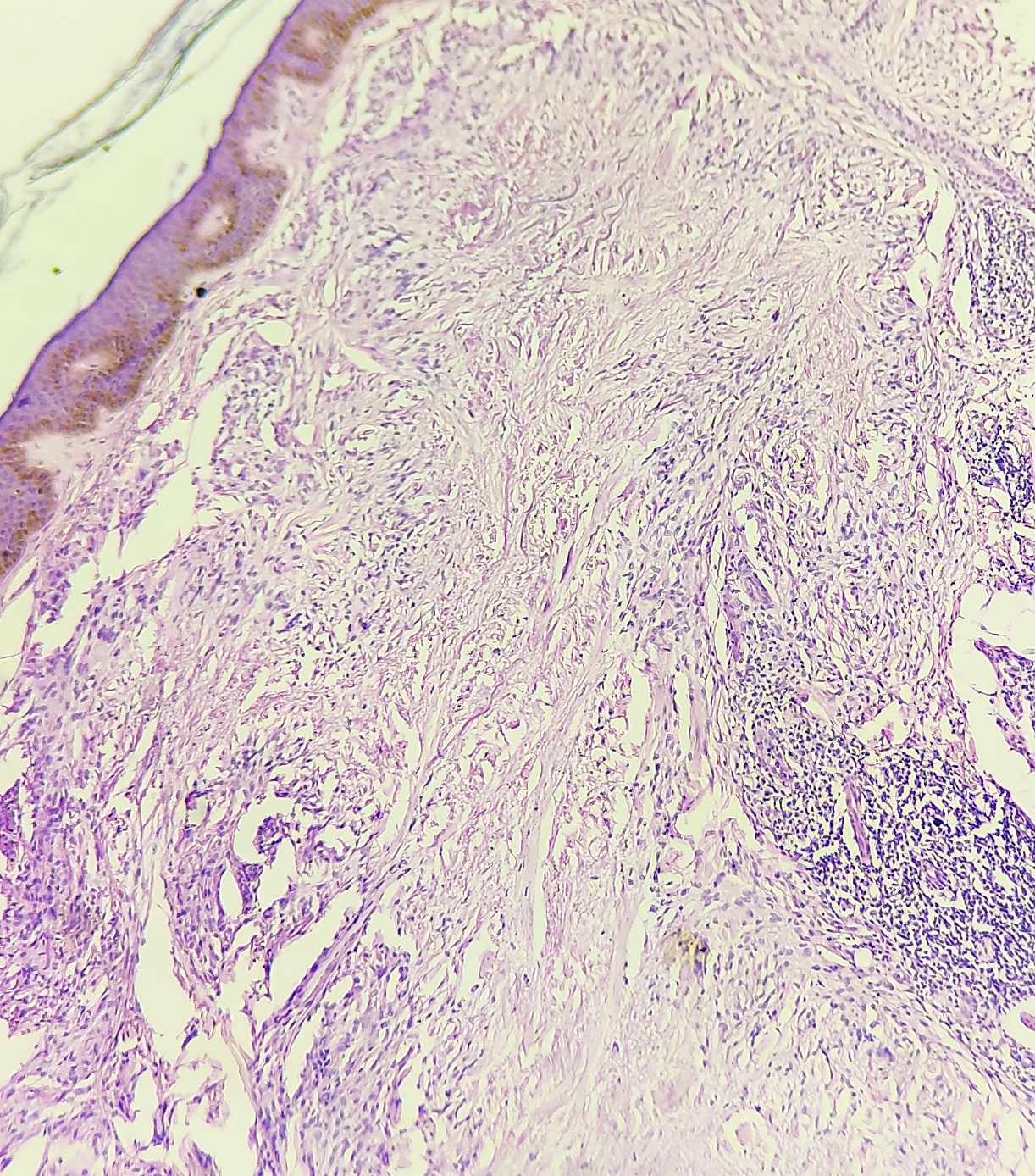
Annular elastolytic giant cell granuloma was seen in 14% of the total cases studied. Microscopy showed scattered ill-defined granuloma along with foci of necrobiosis and palisading histiocytes surrounding the degenerating collagen fibres. Elastophagocytosis was identified in our cases (Figure 3, Figure 4).
Histologically, 3 cases (9%) of perforating folliculitis showed foci of granulomatous infiltrate with adjacent areas showing a mixed perifollicular lymphocytic infiltrate composed of neutrophils, lymphocytes and histiocytes.
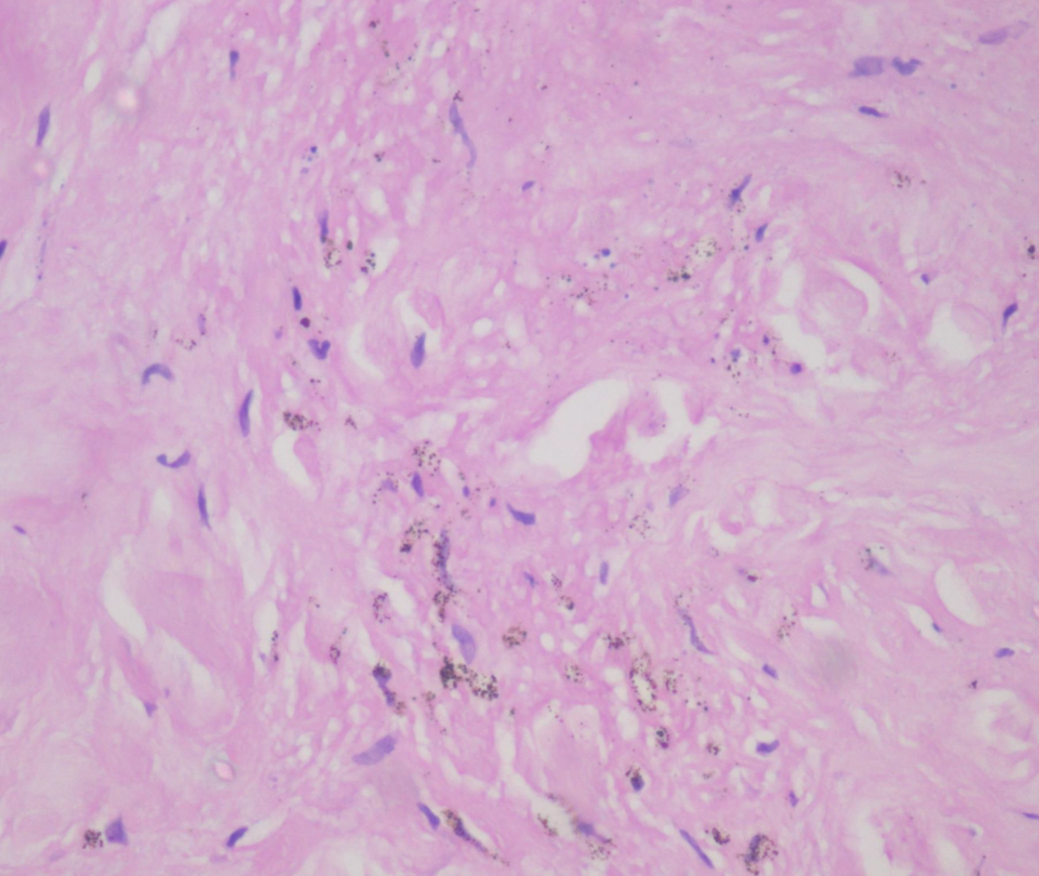
Tattoo granulomas were noted predominantly in male patients and seen in 9% of cases studied. These cases showed a mixed inflammatory reaction in the dermis composed of epithelioid granuloma. Tattoo pigments were seen within multinucleate giant cells and in extracellular areas of dermis.(Figure 5).
Figure 1
Photograph of granuloma annulare showing lymphohistiocytic infiltrates and foci of degenerated collagen (H&E 200X)

Figure 2
Photograph of Granuloma annulare with lymphocytic inflammatory infiltrates and giant cells(H&E 400X).
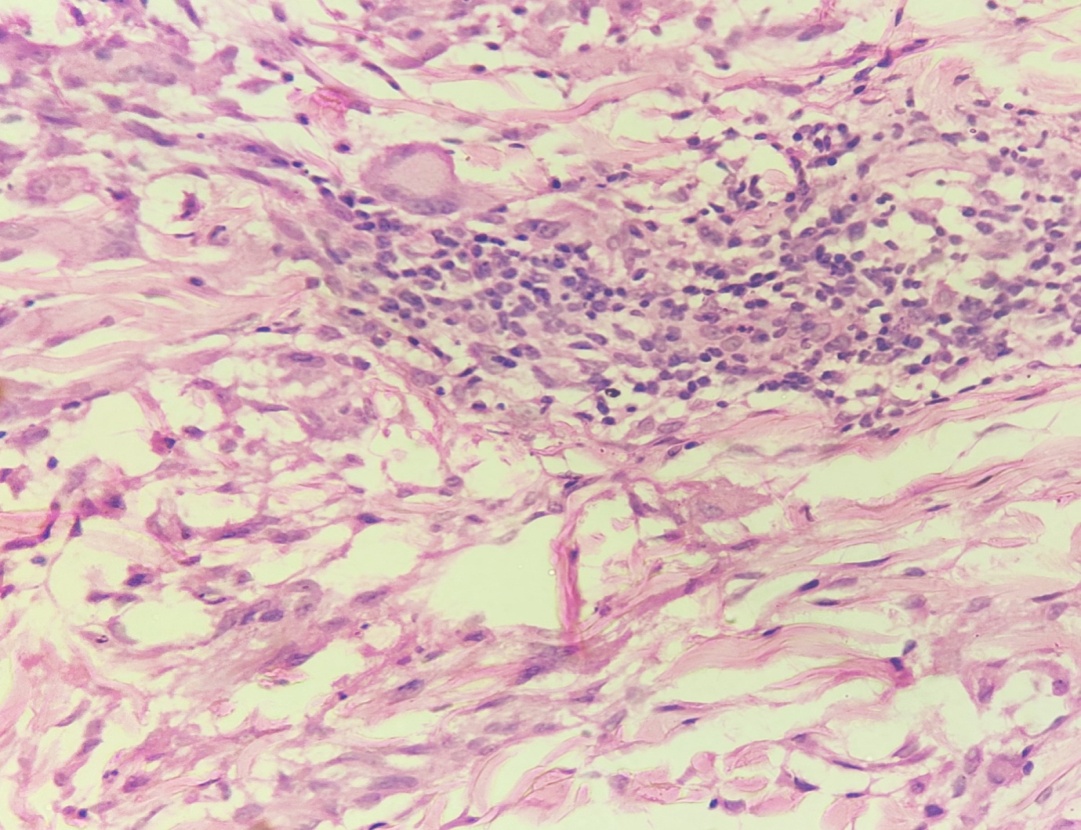
Figure 3
Photograph of Annular elastolytic giant cell granuloma showing elastic degeneration (H&E 200X)
Discussion
Non-infectious granulomatous disorders of skin encompass a large group of disorders which shows overlapping clinical and histological features. The diagnosis and counselling patients regarding their prognosis become challenging. This study has documented the histopathological profile of non-infectious granulomatous dermatoses in a tertiary care centre. The sex distribution pattern revealed that most of the patients were females (71%) with male to female ratio being 1:2.4. Whereas in study conducted by Mohan et al. and Grover et al. there was male predominance.3, 4
In the present study, non-infectious granulomatous dermatoses were found only in 6% of total granulomatous lesions. However, in a study conducted by Gautham K et al., it constituted about 25.5% of cases.5 Granuloma annulare accounts for 50% of all non-infective granulomas in our study. This finding of granuloma annulare being the most common non-infective granulomatous lesion is consistent with findings from similar studies conducted by Grover et al., in which it constituted 78.57% of their study population.3 However, in a study conducted by Mohan et al, granulomatous skin lesions caused by sarcoidosis constituted a majority of their cases, which was found to be a part of systemic manifestation of the disease.4 The increased incidence of granuloma annulare could be attributed to its association with a myriad of diseases which includes diabetes, dyslipidemia, thyroid disease, HIV etc.6, 7
Annular elastolytic giant cell granuloma was noted in 14% of 34 cases in our study, which is similar to the study done by Grover et al where it constituted 10.3% of 29 cases. It was characterized by elastin degeneration, multinucleate giant cells and elastophagocytosis which were similar to the histopathological finding in a study done by Arora s et al.8
Out of 34 cases studied, 9% were each of Foreign body granuloma and Tattoo granuloma, whereas Gautam K et al noted foreign body granuloma in 18.9% of cases which were associated with epidermal cyst.5 Mohan et al. identified 14% foreign body granuloma in their study. Due to increased social acceptance of body inking and tattooing, the tattoo epidemic is on the rise in India. This may present as a granulomatous reaction which is a great mimicker of other granulomatous disorder.9 This granuloma formation may be the result of an excessive immune response to endogenous or exogenous substances. A foreign body or tattoo pigment can be seen histopathologically.
Xanthogranuloma was noted in 9% of cases in our study whereas in study conducted by Mohan et al it was identified in 4.2% of 71 cases. Both Xanthoma and Xanthalesma are characterized by localized infiltrates of the lipid-laden macrophages appearing on various areas of the skin or visceral organs. In our study these lesions were predominantly seen around eyelids. It may represent as a localized idiopathic cutaneous phenomenon or maybe a sign of systemic hyperlipidemia and thus knowing the lipid profile of the patient is important to exclude systemic disease.10
A miscellaneous group which may show rarely granulomatous lesion like perforating folliculitis was found in three cases which showed dilated infundibulum filled with keratin along with foreign body granuloma.
In our study, histopathological features of various non-infectious granulomatous dermatoses were studied. Due to the limited incidence of these lesions, not many literatures were available to compare the incidence, demographic factors and histopathological variation among patients in different parts of the world.
Conclusion
Granulomatous skin lesions have various modes of presentation with both infectious and non-infectious etiology. There is a significant overlap in morphology and clinical presentation and so it is necessary to highlight or observe subtle findings which help in differentiating between various granulomatous dermatoses. Morphology alone is seldom specific and cannot be used as a diagnostic tool for identification of specific diseases. Thus, adequate clinical data and work up in the combination of pathological resources with ancillary techniques can help in elucidation of specific diagnosis and better management of the patients.