Introduction
Thyroid diseases are among the commonest endocrine disorders worldwide with about 42 million people in India suffering from them.1 Fine needle aspiration cytology (FNAC) is the first line diagnostic procedure for evaluating thyroid lesions and can effectively distinguish between neoplastic and non‑neoplastic lesions.2 Most thyroid nodules are benign and a benign result is the most common FNA interpretation (approximately 60-70% of all cases).3
Chronic lymphocytic thyroiditis is the second most common benign thyroid FNA diagnosis next to benign follicular nodule,2, 4 and also overall the second most common thyroid lesion diagnosed on FNAC after goitre.5 Hashimoto’s thyroiditis (HT), a synonym for chronic lymphocytic thyroiditis or autoimmune thyroiditis is more common in women and has prevalence rate of 1–4% and incidence of 30–60/100000 population per year.5 FNA is highly sensitive in diagnosing HT, with a diagnostic accuracy rate of 92%.6 Most patients present with painless enlargement of thyroid, usually symmetric and diffuse. It is the most common cause of hypothyroidism in iodine sufficient areas of the world.7 Besides FNAC, clinical features, thyroid antibody titres, thyroid hormonal profile, and ultrasonography also help in its diagnosis.6, 8
The present study was carried out to evaluate thyroid fine needle aspirates for cytological features of lymphocytic thyroiditis; to grade lymphocytic thyroiditis cases based on predefined cytological criteria and to correlate cytological grades with thyroid hormonal status.
Materials and Methods
It was a three year retrospective study conducted in the Department of Pathology, Government Medical College, Jammu. Thyroid fine needle aspirates from patients presenting with thyroid swelling during this period were retrieved from the archives of our department. May-Grunwald-Giemsa (MGG) and Papanicolaou (PAP) stained smears from these patients were examined under light microscopy.
Cytomorphological features were assessed as per Bethesda system and the cases that were composed of many polymorphic lymphoid cells associated with benign thyroid follicular cells and/or Hurthle cells were reported as lymphocytic thyroiditis (LT) as per The Bethesda System for Reporting Thyroid Cytopathology. A minimum number of follicular or Hurthle cells for adequacy were not required for diagnosis of lymphocytic thyroiditis.3
These cases were further graded based on predefined cytological criteria as per Bhatia et al.8 as:
Grade 0- No lymphoid cells.
Grade I (Mild)- Few lymphoid cells infiltrating the follicles/increased number of lymphocytes in the background.
Grade II (Moderate)- Moderate lymphocytic infiltration or mild lymphocytic infiltration with Hurthle cell change/giant cells/anisonucleosis.
Grade III (Severe)- Florid lymphocytic inflammation with germinal center formation, very few follicular cells left.
Thyroid hormonal profile of these patients, wherever available, was evaluated. The patients were classified as euthyroid, hypothyroid and hyperthyroid based on their serum TSH, T4 and T3 values. Cytological grades were compared with thyroid hormonal status wherever available. Statistically, the association of grades with hormonal status was assessed using Fischer Exact test of significance and P value < 0.05 was considered as statistically significant.
Results
A total of 162 cases of lymphocytic thyroiditis were reported as per Bethesda system in our study. Most patients were in 31-40 years (48; 29.63%) age group followed by 21-30 years (36; 22.22%) and 41-50 years (32; 19.75%) age groups. Mean age was 35.99 years with age ranging from 7 to 80 years. The study had 146 (90.12%) females and 16 (9.88%) males with female to male ratio of 9.125.
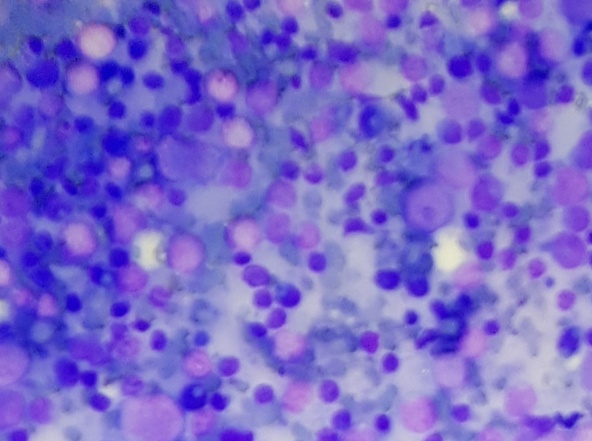
These cases were further graded as per Bhatia et al criteria. Maximum number of cases were of grade II thyroiditis followed by grade I and grade III (Table 1) (Figure 1, Figure 2, Figure 3).
Table 1
Distribution of lymphocytic thyroiditis cases into cytological grades
| Lymphocytic thyroiditis - cytological grading | No. of cases | Percentage |
| Grade I (Mild) | 48 | 29.6% |
| Grade II (Moderate) | 104 | 64.2% |
| Grade III (Severe) | 10 | 6.2% |
| Total | 162 | 100% |
Out of 162 cases, thyroid hormonal profile was available for 78 cases. Maximum patients were hypothyroid (42; 53.85%) followed by euthyroid (21; 26.92%) and hyperthyroid (15; 19.23%). Cases with elevated TSH but normal T4 and T3 were considered as having subclinical hypothyroidism (11; 14.10%).
Cytological grades were compared with thyroid hormonal status as shown in Table 2. Majority of patients with grade II thyroiditis were associated with hypothyroidism. Most of the euthyroid cases were associated with grade II thyroiditis followed by grade I thyroiditis and none with grade III thyroiditis. No patient with grade III thyroiditis with available thyroid profile had normal hormonal status. The lymphocytic thyroiditis cases with hyperthyroidism (Hashitoxicosis), most were having grade II (8 cases) followed by grade I (6 cases) thyroiditis with only 1 case with grade III thyroiditis (Table 2). However, the correlation between cytological grades and thyroid hormonal status of the patients was not statistically significant (P value = 0.21 i.e. > 0.05).
Table 2
Comparison of cytological grades with thyroid hormonal status
| Cytological grade | Euthyroid | Hypothyroid | Hyperthyroid | Total |
| Grade I | 8 | 8 | 6 | 22 |
| Grade II | 13 | 32 | 8 | 53 |
| Grade III | 0 | 2 | 1 | 3 |
| Total | 21 | 42 | 15 | 78 |
Figure 1
Photomicrograph from a case of grade I lymphocytic thyroiditis showing a cluster of thyroid follicular cells infiltrated by few lymphocytes (MGG 400X).

Discussion
The first report of chronic thyroiditis, struma lymphomatosa was described by Hakaru Hashimoto in 1912, which bears his name.8 Hashimoto's thyroiditis is an autoimmune disease that results in destruction of thyroid gland and gradual and progressive thyroid failure.7 The incidence of HT seems to be increasing in the recent times. It has become 10 times more common than it was until the early 1990s. This increase in incidence has been linked to excess iodine intake, particularly in coastal areas.9, 10
Cytological findings of lymphoid cells in the background and infiltration of follicular cells by lymphoid cells are characteristic. Variable features include Hurthle cells, plasma cells, epithelioid cell granulomas and multinucleated giant cells.11 In the usual case hypothyroidism develops gradually. In some patients, it may be preceded by transient thyrotoxicosis during which free T4 and T3 levels are elevated and TSH is diminished. As hypothyroidism supervenes, T4 and T3 levels fall with a compensatory increase in TSH.7
Thyroid fine needle aspirates were analysed for cytological features of lymphocytic thyroiditis according to Bethesda system and a total of 162 cases were reported as lymphocytic thyroiditis in the present study. Most common age group of these patients in our study was 31-40 years which is similar to studies by Bhatia et al,8 Anila et al,6 and Shetty et al.12 This younger age of diagnosis of lymphocytic thyroiditis in Indian population as shown by these Indian studies differs from a western study in which median age of subjects was 58 years.13 The present study showed female predominance that is comparable to most studies in literature.5, 6, 8, 12
On further grading, majority patients had grade II thyroiditis followed by grade I thyroiditis with grade III thyroiditis in least number of patients in our study. This is similar to studies by Bhatia et al.8 and Shetty et al.12 However, in a study by Anila et al,6 majority of patients had grade I thyroiditis and in a study by Sood et al.,5 majority cases were of grade III thyroiditis.
On assessing thyroid hormonal status, majority of the patients were hypothyroid similar to many other studies.8, 12, 14 Patients with subclinical hypothyroidism in our study were 11 (14.10%). In a study by Shetty et al.,12 39.6% of the cases presented with subclinical hypothyroidism which is higher than our study. On further correlation of cytological grades with thyroid hormonal status of patients, no statistically significant association was found in our study which is consistent with many studies in literature.6, 8, 12
However, in a study by Sood et al.,5 Grade 3 lymphocytic infiltration has statistical correlation with TPO and TSH together or TSH alone. In a study by Kumar et al.,15 the association between hormonal status and lymphocytic infiltration was statistically significant (P- 0.02). Among cases with moderate to heavy infiltration, the ratio of hypothyroidism (44%) was greater than hyperthyroidism (6%), but no statistically significant association was noted for hypo- or euthyroidism (P- 0.36; P- 0.29). Among cases with minimal infiltration the proportion of hyperthyroid cases was greatest (47%) and statistically significant (P- 0.0006). In a study by Megalamane et al.,16 there was a statistical significance between the cytological grades of LT and TSH (p-value <0.001).
There is an overlap of clinical, radiological and hormonal parameters in Hashimoto's thyroiditis and other thyroid lesions, and thus are not very helpful.15 In equivocal cases antibody testing is helpful, but about 7 to 33% cases of Hashimoto's thyroiditis are antibody negative particularly in initial phase of the disease due to local antibody production by intrathyroidal lymphocytes without spill over into the blood.11, 16 FNAC is thus considered superior as well as more cost-effective than antibody screening to diagnose Hashimoto's thyroiditis,10, 17 in initial stage of disease and if antibody testing facilities are not available as in our institution or are not affordable due to high cost.15
However, FNAC has certain pitfalls in diagnosing lymphocytic thyroiditis. Diagnosis of Hashimoto's thyroiditis is likely to be missed in smears showing cytological evidence of hyperplasia as in Grave's disease or abundant colloid.9 Distinction between Hashimoto's thyroiditis in toxic phase i.e. Hashitoxicosis and pure Grave’s disease may not be possible cytologically and require correlation with clinical details and hormonal profile.11 Smears showing hyperplastic follicular cells, Hurthle cells, a limited population of lymphocytes in the background but absence of lymphocytes in epithelial groups poses a major diagnostic problem, with adenomatous/colloid/hyperplastic goitre as the main differential diagnosis in I2 deficient regions.15
In early stages of Hashimoto thyroiditis, selective sampling from hyperplastic nodule comprising predominantly of Hurthle cells with sparse or absent lymphocytic infiltrate raises the suspicion of Hurthle cell neoplasm.3 Hurthle cells in flat sheets favor thyroiditis while poorly organized, and poorly cohesive cell clusters favor neoplasia.11 Predominance of lymphoid component as in grade III thyroiditis may raise the possibility of lymphoma.12 About 75% of primary lymphomas of thyroid gland arise in a background of Hashimoto's thyroiditis.11 The polymorphic lymphoid population helps in distinguishing these cases from Non-Hodgkin lymphoma.3, 8 Immunophenotyping studies are essential to confirm its diagnosis in morphologically equivocal cases. The incidence of malignancy in HT is documented to vary from 0.4% to 28%. The follicular or Hurthle cells in LT occasionally show mild atypia, nuclear enlargement, grooves and chromatin clearing, therefore possibility of papillary carcinoma should be slightly raised.3, 12
Thus, being aware of overlapping cytological features with other thyroid pathologies, and by following an integrated approach with clinicopathologic correlation, some of the potential pitfalls and uncertainties can be minimized and the value of FNAC in the diagnosis of lymphocytic thyroiditis can be enhanced.
Conclusion
Though a combination of cytomorphology, clinical features, thyroid hormonal profile, antibody testing and ultrasonographic features help in the diagnosis of lymphocytic thyroiditis particularly in cytologically equivocal cases, FNAC remains the "gold standard" investigation for diagnosis of lymphocytic thyroiditis similar to other studies.5, 6, 8, 10, 12, 14 However, the cytological grades show no statistically significant correlation with thyroid hormonal status in our study.