Introduction
Lungs are one of the vital organs in body and participate in exchange of gases between inspired air and blood.1, 2 Millions of people around the world suffer from preventable chronic respiratory diseases, which are based on various factors such as age, sex, socioeconomic status, food habits, lifestyle, locality, associated infections and endemic diseases.2, 3, 4, 5, 6, 7
Lungs are common organs involved in various types of inflammation, non-neoplastic, neoplastic, occupational and other diseases.2, 3, 4, 5, 6 Lungs are secondarily involved in almost all forms of terminal events in cardiovascular diseases and also common site for metastasis.1, 2, 3, 4, 5, 6
The clinical and radiological findings in pulmonary diseases are nonspecific, hence prompt pathology investigations and diagnosis are essential to improve patient’s survival and reduce further morbidity and mortality.2, 4, 5
Pathological examination of autopsy specimen of lungs gives valuable information and improves clinical diagnosis in spite of modern technologies.3, 4, 5 But over the years autopsy rates have declined mainly owing to modern medical technology building false confidence, economic burden, fear of litigation and attitudinal change.6, 8 So, the present study was taken to identify the spectrum of histopathological alterations in lung specimens, irrespective of cause of death and sex.
Materials and Methods
Source of data
One hundred fifteen autopsy specimens of lungs of individuals above 18 years of age irrespective of cause of death from the Department of Forensic Medicine, Belagavi Institute of Medical Sciences, Belagavi were included. Cases collected during the period from November 2015 to June 2017 (18months) were taken for the study.
Inclusion criteria
Lung specimens from cases above 18years of age, with irrespective of cause of death were taken.
Methods
One hundred fifteen autopsy specimens of lungs of individual above 18 years irrespective of cause of death were collected from the Department of Forensic Medicine, Belagavi Institute of medical sciences, Belagavi were taken for the study. Clinical history and autopsy findings were noted down from the autopsy records. Lungs were removed according to standard autopsy technique and fixed in 10% formalin. Detailed gross examination was done and minimum of one section from each lobe of lungs were taken and more sections were given in grossly visible lesions. Sections were routinely processed and stained with Hematoxylin and Eosin. Detailed histopathological examination was done. Special stains like Ziehl-Neelsen (ZN), Periodic acid-Schiff (PAS), Reticulin stain and Pearls stain were done wherever necessary.
Results
A total of 115 lung specimens of individual above 18 years of age, irrespective of cause of death were studied.
In 107 cases, 106(99.06%) showed non neoplastic lesions and one specimen (0.94%) showed neoplastic lesion. In the present study males to females with a ratio of 3.4:1. Males constituted 89 cases (77.4%) and females 26 cases (22.6%).
The most common age group for both males and females was 20-29 years (26.9%) followed by 40-49 years(19.1%). Males-20 cases (64.5%), Females-11 cases(35.4%).
Table 1
Sex-wise distribution of lesions
All Non neoplastic lesions were common in males. Granulomatous lesions were common in females. In Non neoplastic lesions, grossly visible lesions of lungs were seen in 33 cases (31.13%) and 73 cases (68.8%) were unremarkable.
In the present study, more than one morphological pattern was seen which is more in left lung 36 cases (33.9%) compared to right lung (29.2%). The most common combined lesion was pulmonary edema with pulmonary congestion 7cases (6.5%).
Single lesions like tuberculosis was more common in right lung 5 cases (4.71%). Chronic venous congestive changes were more in left lung 5 cases (4.71%). Lobar pneumonia was common in left lower lobe 4 cases (3.77%). Emphysema changes were common in left upper lobe 3 cases (2.8%). Granulomatous lesions were common in left upper lobe 2 cases (1.88%).
ZN stain was done for 08 cases, only 2 cases showed acid fast bacilli (1+ and 2+).
One case of honey comb lung also known as End stage of Chronic Interstitial lung disease which showed obliteration of bronchioles by fibrosis and compensatory dilatation of neighbouring bronchioles, which forms the honeycomb appearance.
One case of amniotic fluid embolism was reported in a 29 year female, who had postpartum bleeding.
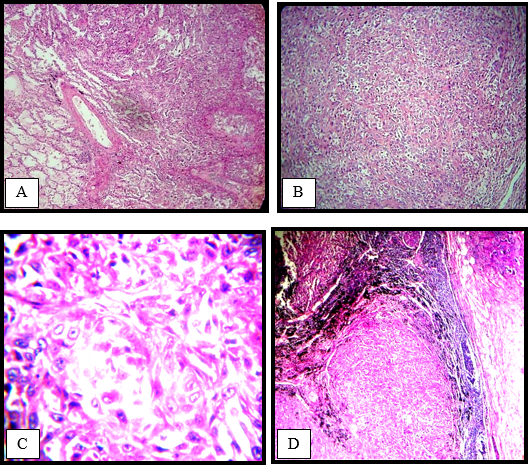
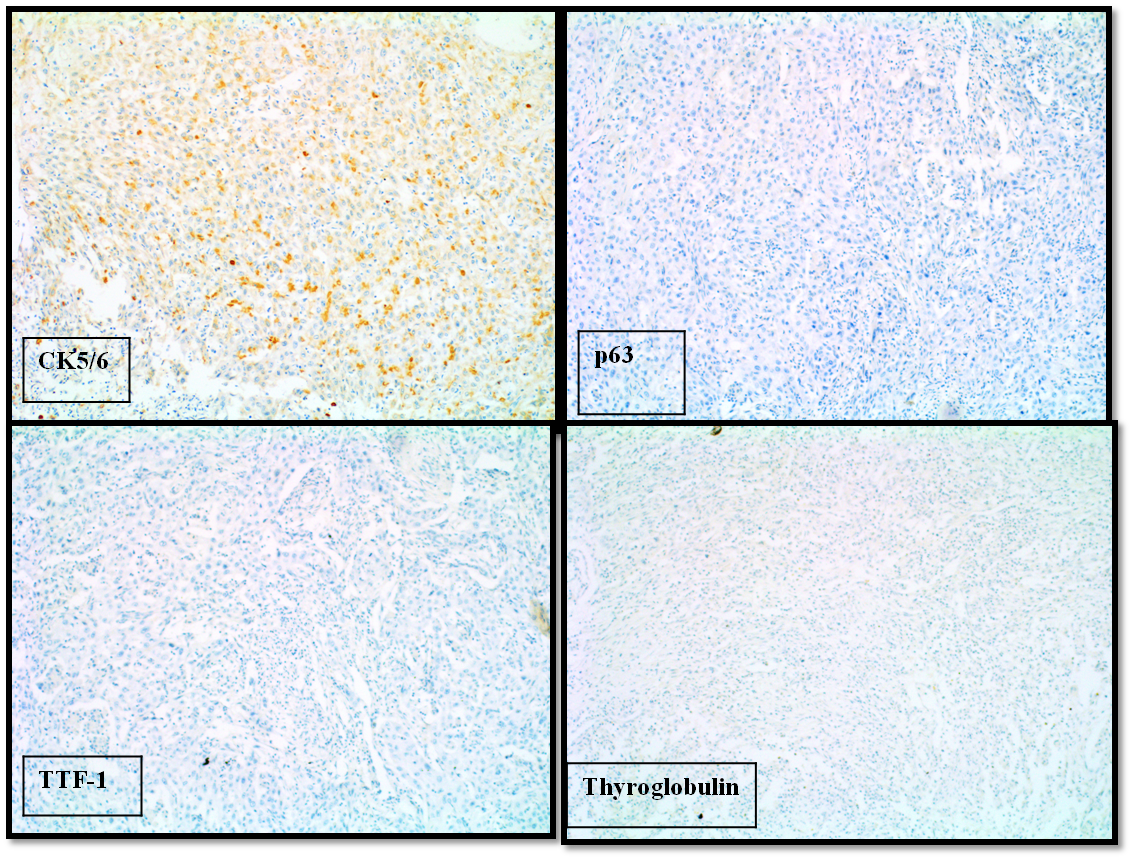
In the present study only one case of neoplastic lesion in a 47 year female, who had thyroid malignancy was reported. Grossly, both lungs showed grey-white, firm nodules both on outer surface and cut surface. Microscopically, it was diagnosed as bilateral metastatic undifferentiated carcinoma. IHC was done.
Tumor tissue showed positivity only for CK5/6 and negative for various IHC markers like CK 20, TTF-1, thyroglobulin, Vimentin, calretinin and NSE. Finally a diagnosis suggestive of poorly differentiated squamous cell carcinoma was made.
In the present study, Hilar lymph nodes were received in 60 cases (52%). Out of 60 cases 43 cases (71.6%) were unremarkable, 14 cases (23.3%) showed reactive lymphadenitis, 2 cases (3.3%) showed granulomatous lymphadenitis and one case (1.6%) showed metastasis.
Cause of death was known in 97 cases (90.65%) of pathological lesions. Road traffic accident (RTA), 28 cases (26.2%) was the most common followed by sudden death (15.9%). RTA was common in males. History of lung disease was present in 4 cases (3.7%) where 3 cases had history of tuberculosis. One case was HIV positive.
Figure 4
Microphotograph of amnioticfluid embolism showing; a): Anucleate squames in pulmonary vessel (arrow) (H& E x 100); b): Higher magnification of the same (arrow) (H& E x 400)
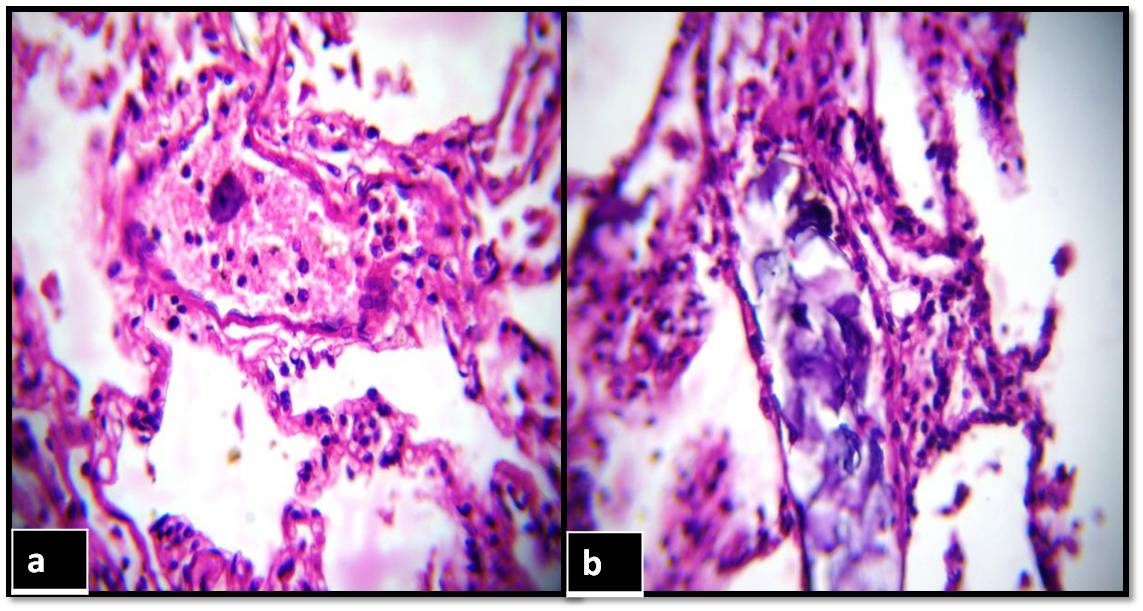
Figure 5
Shows honeycomb lung showing; a): Cobblestone appearance (arrow); b): Cut surface; c): Microphotograph of honeycomb lung showing metaplastic bronchial epithelium, dilated alveoli and peribronchial fibrosis (H & E x 400); d): Black coloured reticulin fibers of interstitial and peribronchial fibrosis (Reticulin stain x 100)
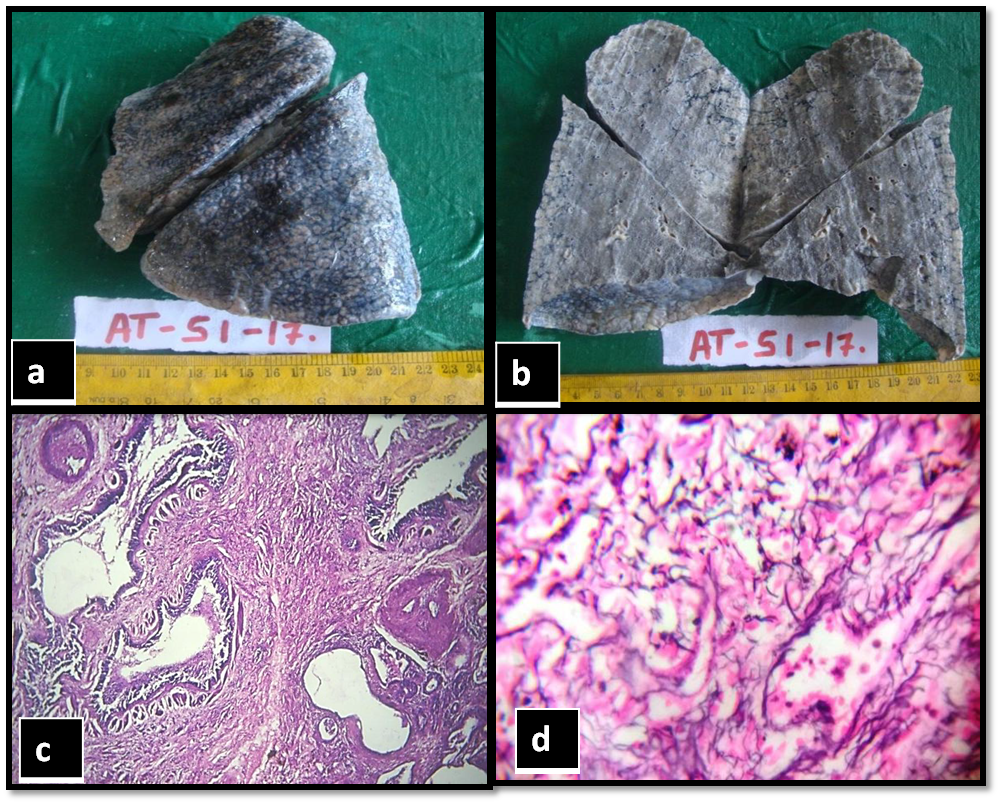
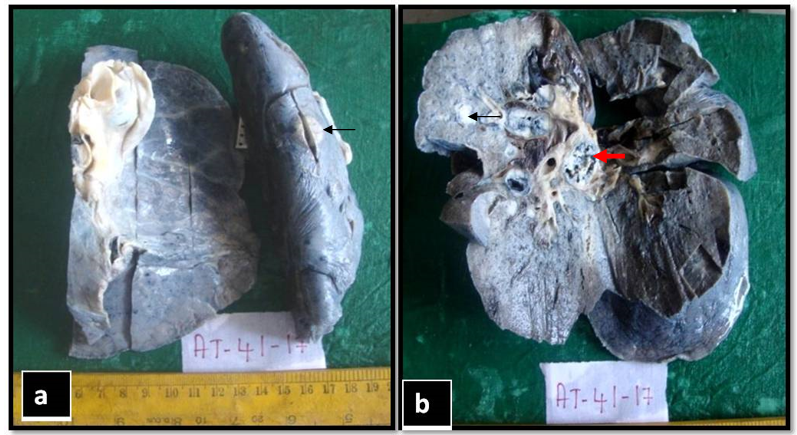
Figure 6
Gross photograph of metastatic carcinoma of lung showing a) outer surface metastatic nodule on left lung (black arrow); b): Cut section showing grey white nodules (arrow) and metastatic hilar lymph node (red arrow)
Discussion
In the present study, pathological lesions were seen in 107 (93.04%) cases. 106 cases showed Non neoplastic lesions (99.06%) and neoplastic lesion in 1 case (0.093%).
According to Selvam et al7 pathological lesions were seen in 108 cases (90%) out of 120cases and study done by Mangal et al2 showed lesions in 1549 cases (90.32%) out of 1715 cases.
In the study done by Tahir et al4 carried out on 810 specimens of the lungs, out of which 648 cases (80%) showed pathological lesions. Chauhan et al5 conducted study on 335 lung specimens, pathological lesions were sen in 285 cases (85.1%). 5 Findings of our study are in concordance with Selvam et al, 7 Mangal et al, 2 Tahir et al4 and Chauhan et al.5
Distribution of pathological lesions
In the present study, 106 cases showed Non neoplastic lesions (92.2%) and neoplastic lesion in 1 case (0.87%) which was similar to study done by Mangal et al.2
Table 2
Comparison of distribution of lesions with various other studies
| Chauhan G et al5 | Mangal K et al2 | Bal MS et al6 | Present study | |
| Non- neoplastic | 82.9% | 90% | 78% | 92.2% |
| Neoplastic | 2.08% | 0.41% | 2% | 0.87% |
Table 3
Comparison of spectrum of Non neoplastic lesions in various studies
Sex wise distribution of lesions
In the present study, lesions were more in males (77.4%) compared to females (22.6%). It is comparable to study done by Mangal et al2 (76.09%), Udayashankar et al3 (77.2%), Chauhan et al5 (71.64%) and Selvam et al 7 (75.9%) The difference between males and females was significant (Chi-square = 36.26 & p<0.001).
Males were more affected in the present study as males are vulnerable for various diseases due to exposure of occupational risk factors and also due to addiction to smoking and alcohol.
In the present study majority of cases were in the age group 20-29 years (28.9%) followed by 40-49 years (20.5%) which was similar to that of Mangal et al2 (45.6%)
In the present study, more than one morphological pattern was seen in 48 cases (44.8%). Among these, most common pattern was pulmonary edema with pulmonary congestion in 7 cases (6.6%). Studies done by Khare et al9 and Mangal et al2 showed pulmonary edema with pulmonary congestion 24 cases (42.86%) and in 1325 cases (77.26%) respectivel.
Conclusion
Non neoplastic lesions were common in the present study and males were commonly affected. More than one histomorphological change was seen in majority of the cases and our study confirmed the diagnosis of amniotic fluid embolism and metastatic lung cancer. Hence to conclude, autopsy studies in lungs should be done by taking large sample of cases which will broaden the range of histopathological lesions and give much more accurate estimate of frequency of different types of lesions in lungs.