Introduction
Pancytopenia refers to a decrease in all the three cell lines of blood viz. RBCs, WBCs and Platelets, while bicytopenia refers to reduction in any two out of the three. Pancytopenia is diagnosed when the hemoglobin (Hb) <10g%, absolute neutrophil count (ANC) <1.5 x 109/L and platelet count <100 x 109/L. It is labelled severe if patient has two or more of the following: Hb <7 gm%, ANC <0.5 x 109/L, and platelet count <20 x 109/L.1 Pancytopenia has a wide etiological profile, ranging from simple drug-induced bone marrow hypoplasia, nutritional deficiencies to fatal bone marrow aplasia and leukemia. Identification of correct cause is mandatory as it will help in implementing appropriate therapy and assessing the prognosis.2 Etiological classification of pancytopenia can be done into three groups- failure of production (implying intrinsic bone marrow disease), sequestration (hypersplenism), and increased peripheral destruction.3
Failure of bone marrow can be due to primary production defects. Primary or genetic causes include Fanconi anemia, dyskeratosis congenita, Shwachman-Diamond syndrome, and amegakaryocytic thrombocytopenia.4 The production of hemopoietic cell can also be prejudiced in the bone marrow either by infections, toxins, and malignant cell infiltration leading to hypocellular marrow.5
When pancytopenia is associated with organomegaly and lymphadenopathy, the possibility of malignancies or bone marrow failure syndromes are considered. There are a number of other causes which can present in the similar way.6
Acquired causes of pancytopenia can be nutritional deficiencies, idiopathic or secondary to exposure to radiation, drugs and chemicals (chemotherapy, chloramphenicol, sulfa drugs, antiepileptics, gold etc), viral infections (cytomegalovirus, Epstein-Barr virus, hepatitis B or C, HIV etc.), auto-immune, paroxysmal nocturnal hemoglobinuria, and marrow replacement disorders (leukemia, myelodysplasia, myelofibrosis).7 Megaloblastic anemia and infections such as enteric fever, malaria, kala-azar and bacterial infections are the common causes of pancytopenia in developing countries.8
Hypersplenism causes pancytopenia by splenic sequestration and in some cases by hemolysis.9 The common causes of hypersplenism include cirrhosis, congestive heart failure, and malignancies like leukemia/lymphoma, hemoglobinopathies and infections.
Autoimmune-mediated disorders like systemic lupus erythematosis (SLE) can present with pancytopenia when all the three cell lines are affected. Patients with autoimmune disorders like rheumatoid arthritis, psoriasis and SLE are at increased risk for lymphoproliferative disorders and it is important to exclude underlying malignancies like lymphoma while evaluating these patients.10, 11, 12 Autoimmune cytopenias are also seen in autoimmune lymphoproliferative syndrome (ALPS) and common variable immunodeficiency disease (CVID).
Paroxysmal nocturnal hemoglobinuria and hemophagocytic lymphohistiocytosis can cause both impaired production and increased peripheral destruction of blood cells.
The aim of this study is to describe the different aetiologies of bicytopenia and pancytopenia in paediatric patients based on clinical and haematological profiles including peripheral blood and bone marrow examination.
Materials and Methods
This descriptive study was undertaken for a period of 6 months (analysis of cases from January 2015-December 2016) at a tertiary care center in central Kerala. All cases of paediatric pancytopenia and bicytopenia with age <12 years based on complete blood count and admitted in the institute during 2 year period from January 2015-December 2016 were taken for the study. Patients beyond these age limits, previously diagnosed cases of aplastic anaemia and leukemia, cases with clinical suspicion of genetic or constitutional pancytopenia, patients with history of blood transfusion in the recent past, and those who were not willing for admission were excluded.
A systematic review of clinical findings provided in the request forms submitted in the lab was done. Complete blood counts(CBC), peripheral smear and bone marrow findings in each case were recorded. Hematological profile(CBC) included hemoglobin, red cell indices, total and differential leukocyte counts, platelet count, peripheral blood smear morphology and bone marrow aspiration/biopsy. Blood counts were done on automated hematology analyzer (sysmex). Platelet counts obtained from counter were confirmed by peripheral blood smear examination. Bone marrow aspiration and trephine biopsy stained with Leishman and hematoxylin and eosin stain respectively, along with special stains were reviewed in cases where they were done. Cytopenia was defined as: hemoglobin < 10g/dL, total leukocyte count < 4 × 109/L and platelet count < 100 × 109/L and adjustments for age were made wherever necessary. Follow up of patients with CBC and peripheral smear was attempted. The data was entered in Microsoft excel and further statistical analysis was done using IBM SPSS software statistics 20 trial version.
Results
Age group most commonly affected in our study was 9-12 years. Cytopenia affected females more than males (M:F-0.9:1). Most of the children presented with fever and the most common clinical findings were fever, pallor and organomegaly. Hepatomegaly was the most commonly elicited sign (Table 1).
Infections were found to be the major cause of bi/pancytopenia in children who needed hospital admission (Table 2). Dengue fever constituting 34% of the cases was the most common type of infection requiring inpatient care. Second most common cause of bi/pancytopenia was acute leukemia followed by aplastic anemia. No specific identifiable causes were noted in 10 out of 117 cases.
In our study, Bicytopenia cases outnumbered Pancytopenia cases (82 cases vs 35cases). Among bicytopenia cases, combination of anemia and thrombocytopenia was seen in maximum cases followed by anemia and leukopenia. Acute leukemia presented as either bicytopenia or pancytopenia in 30 cases of which majority were bicytopenia (70%).
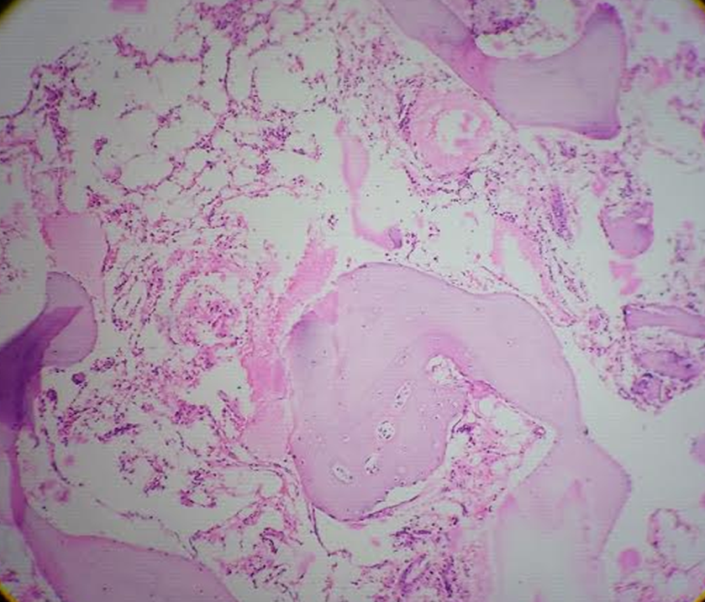
Bone marrow study was done in 63 out of 117 cases, out of which acute leukemia (25.8%) was the most common diagnosis. Acute lymphoblastic leukemia constituted the maximum number (22.2%) of cases among acute leukemia (Figure 1).
Figure 1
Bone marrow aspirate (2639/16) showing blasts in a 3 year old female child with acute lymphoblastic leukemia (Leishman stain, 100X)
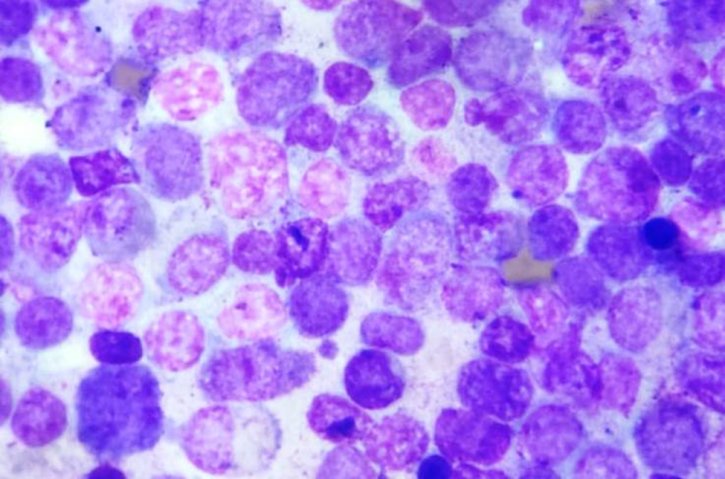
Figure 3
Peripheral smear (4996/16)-11 year old male with hereditary spherocytosis (Leishman; 40X and 100X)

Table 1
Clinical presentation - signs and symptoms
Table 2
Etiological profile of bi/pancytopenia
Discussion
Age group most affected in our study was >9 years. Different studies showed marked variation in the age groups affected which emphasized the lack of correlation between age affected and cytopenia.
Females were affected by cytopenia more than males in our study (0.9:1) which was comparable with the study done by Dubey S et al (0.88:1).13 Many studies showed male predominance, which may be due to variations in the inclusion criteria applied.
Most common presenting symptom was fever (67.52%) which was comparable with studies done by Dubey S et al(68%),13 Rathod GB et al(65%),14 Jan A et al(62.85%),15 Memon S et al(65%)16 and Khan FS et al(68%).17 Hepatomegaly was the most commonly elicited sign(28.21%), similar to the study by Sharif M et al with hepatomegaly seen in 27.6% of cases18 (Table 3).
Most common bicytopenia seen in our study was anemia and thrombocytopenia, with similar findings reported in studies by Dosi S et al19 and Varma N et al20 (Table 3). Bicytopenia could be due to significant marrow disease as in cases of acute leukaemia or due to 2 different pathological processes occurring together. Therefore it is essential to differentiate between the two and identify those cases which need urgent investigations and treatment. In our study, bicytopenia due to anaemia and thrombocytopenia was coexisting nutritional deficiency and viral infections.
The proportion of acute leukemia in bicytopenia and pancytopenia in our study was comparable with the studies by Dosi S et al19 and Waris R et al.21
We observed that the most common cause of cytopenia in our study was infections followed by acute leukemia and aplastic anemia. Most of the studies showed the common causes as megaloblastic anemia and aplastic anemia followed by acute leukemia. This difference could be due to the fact that we included only hospitalized patients with cytopenia. In addition to marrow diseases, those severe infections like dengue fever (34%) warranted hospital stay and hence was included in our study.
Table 3
Comparison of various studies done on paediatric bi/pancytopenia
Limitations of the Study
Infections prevalent at the particular time of season requiring hospital admissions might have contributed more number of cases leading to a bias in the study.
Conclusion
Bicytopenia and pancytopenia in children indicates significant underlying pathology and in our study the most common aetiologies were infections, followed by acute leukemia and aplastic anaemia. Bi/pancytopenia presenting with fever, pallor and bleeding with organomegaly signify underlying bone marrow disorders /malignancies which warrants thorough work up. Peripheral smear and bone marrow examination help in diagnosing such cases.