Introduction
‘Sinonasal tract’ is a collective term used for nasal cavity and paranasal sinuses.1 The main functions of the sinonasal tract are filtering and humidifying inhaled air. The nasal cavity also has specific olfactory receptors for airborne odorant molecules. The paranasal sinuses additionally have the functions of acting as resonating chambers during speech and reducing the relative weight of the skull.2
These functions lead to exposure of various allergens, pathogens, chemical and physical irritants and other environmental influences. As a result of these multifaceted exposures, various inflammatory conditions, infections and neoplasms can occur in the sinonasal tract.3
Prevalence of sinonasal masses in the general population is 1 to 4%.4 A careful clinical workup including symptomatology, radiological investigations and endoscopy helps to determine a differential diagnosis but histopathology provides the final diagnosis.5 Thus histopathological examination is essential for timely diagnosis and intervention.6
Material and Methods
Th is study was a descriptive cross-sectional study and was carried out in the Pathology department of a tertiary care hospital. Institute Ethics Committee Clearance (IECC) was obtained before start of the study.
The study took 2 years for completion and 122 cases from September 2011 to August 2018 were studied. Cases from September 2011 to August 2016 were part of the retrospective study. The archives of the Department of Pathology provided the paraffin blocks, slides and reports required for the retrospective study. For the prospective study, the formalin fixed tissue specimens were received with a detailed clinical history and radiological findings. Gross findings of the specimens was noted and adequate sections were taken and stained with hematoxylin and eosin. Special stains and immunohistochemical stains were used to confirm diagnosis wherever necessary. Neoplastic lesions diagnosed were classified accordin gly by referring the 2017 WHO classification of tumours of nasal cavity and paranasal sinuses.7
Result
Lesions of the sinonasal tract commonly affected the age group 31-40 years (28 cases, 22.95%) followed by 21-30 years (27 cases, 22.13%). Maximum patients of non-neoplastic cases belonged to 21-30 and 31-40 years age groups (24 cases each, 24.49%). Benign lesions were mostly noted in fourth and seventh decade of life (3 cases each, 23.08%) whereas a high proportion of malignant lesions were reported in 61-70 years age group (4 cases, 36.36%). (Table 1)
Table 1
Age distribution of lesions of nasal cavity and paranasal sinuses
Sinonasal tract lesions were commonly seen in males. 71 out of 122 cases (58.20%) were males and 51 cases (41.80%) were females. Out of the 98 non-neoplastic cases diagnosed, majority were males (61 cases, 62.25%) whereas female preponderance was noted among neoplastic lesions (14 of 24 cases, 58.33%).
Of the total 122 cases included in this study, the non-neoplastic cases (98 cases) outnumbered the neoplastic cases (24 cases). Cases diagnosed as benign lesions (13 cases, 10.66%) were marginally higher than those diagnosed as malignant (11 cases, 9.01%).
In terms of frequency, the non-neoplastic lesions of sinonasal tract diagnosed were, in descending order, sinonasal polyp, fungal rhinosinusitis, epidermal inclusion cyst, rhinosporidiosis, chronic non-specific inflammation, lepromatous leprosy and arteriovenous malformati on (Table 2). Benign lesions comprised of hemangioma, inverted sinonasal papilloma, angiofibroma and trichoepithelioma (Table 3). Squamous cell carcinoma, malignant melanoma, nasopharyngeal carcinoma, adenoid cystic carcinoma and T-cell lymphoma were the malignant lesions noted (Table 4).
Table 2
List of non-neoplastic lesions of sinonasal tract diagnosed in the present study
Table 3
List of benign neoplastic lesions of sinonasal tract detected in the present study
Table 4
List of malignant neoplastic lesions of sinonasal tract detected in the present study
Figure 1
Photomicrograph of sinonasal polyp. Ciliated pseudostratified columnar respiratory epithelium with stromal mixed inflammatory infiltrate. (H&E, 400X)

Figure 2
Photomicrograph of aspergillosis (mycetoma). Aggregates of hyphaenoted. Hyphae are thin and branch at acute angles. (H&E, 400X) Inset: GMS stain highlights the thin, branching hyphae
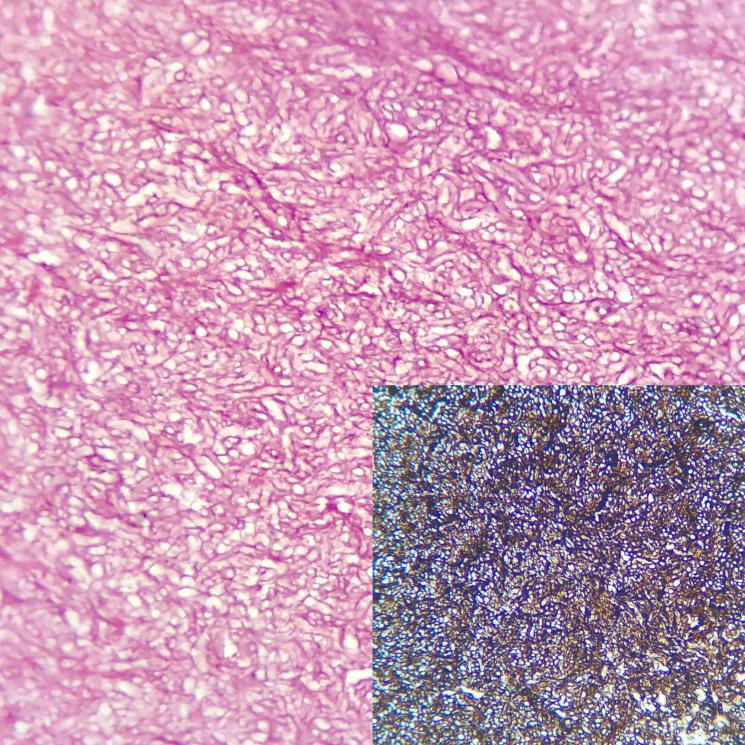
Figure 3
Photomicrograph of rhinosporidiosis. Subepithelial and submucosal sporangia containing sporangiospores noted. (H&E, 100X)
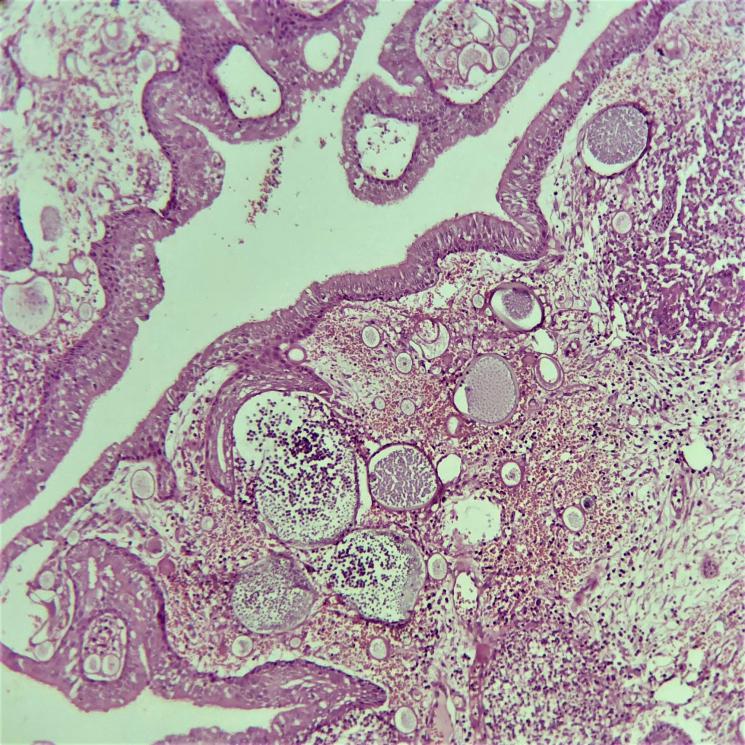
Figure 4
Photomicrograph of capillary hemangioma. Well circumscribed, lobular arrangement with capillary proliferation. Overlying collarette of epithelium is noted. (H&E, 100X)

Figure 5
Photomicrograph of inverted sinonasal papilloma. Surface epithelium showing multiple inversion with loss of seromucinous glands in the submucosa. (H&E, 100X)

Discussion
In the present study, age of presentation showed a wide range from 2 to 90 years. Maximum cases were noted in the fourth decade (28 cases, 22.95%) followed by the third decade (27 cases, 22.13%). Raj et al found maximum cases in third decade (32.79%) followed by fourth decade (21.31%).8 In the study conducted by Mane et al, the most common age group was 21-30 years (35 cases, 27.78%) followed by 31-40 years (31 cases, 24.60%).9
Male to female ratio of 1.39:1 was calculated in this study. Similar findings of male preponderance were observed in studies conducted by Tondon et al,10 Khan et al11 and Kulkarni et al.6
We observed higher frequency of non-neoplastic lesions (80.33%) in comparison with neoplastic lesions (19.67%). Our findings are in concordance with Khan et al,11 Kulkarni et al6 and Mane et al.9 However Dasgupta et al12 recorded an almost equal proportion of neoplastic and non-neoplastic lesions. (Table 5)
Table 5
Frequency of non-neoplastic and neoplastic lesions compared to previous studies
Non-neoplastic lesions of sinonasal tract
In the present study, majority of the lesions were of non-neoplastic etiology. The most common non-neoplastic lesion was sinonasal polyp (85.72%) followed by fungal rhinosinusitis (5.10%), epidermal inclusion cyst (4.08%), rhinosporidiosis (2.04%), lepromatous leprosy (1.02%), chronic nonspecific inflammation (1.02%) and arteriovenous malformation (1.02%). Studies conducted by Dasgupta et al,12 Pushpalatha et al14 and Mane et al9 also noted that sinonasal polyp was the most common non-neoplastic lesion. Other non- neoplastic lesions like fungal rhinosinusitis, rhinosporidiosis and epidermal inclusion cyst showed varying frequencies.
Sinonasal polyps
Peak incidence of sinonasal polyps was noted in the third decade. Similar findings were observed by Khan et al11 and Kulkarni et al6 who reported a peak incidence in second and third decade of life. Male predominance was observed and this was in compliance with the studies by Dasgupta et al12 and Khan et al.11 Microscopically, the epithelial lining is ciliated pseudostratified columnar, with stromal infiltrate comprising of eosinophils, lymphocytes and neutrophils. (Figure 1)
Fungal rhinosinusitis
According to this study, the mean age of presentation of patients diagnosed with fungal rhinosinusitis was 62.4 years wit h female predominance (M:F ratio 1:1.5). Mane et al9 reported the mean age of presentation of fungal rhinosinusitis was 50.7 years with male preponderance (2:1). This suggests that fungal rhinosinusitis mainly affects the elderly. On microscopy, the fungal hyphae were thin and branching at acute angles. (Figure 2)
Neoplastic lesions of sinonasal tract
In the present study, benign neoplastic lesions (54.17%) marginally outnumbered the malignant neoplastic lesions (45.83%). Similar findings were noted in the study by Khan et al.11 But Tondon et al10 and Mane et al9 reported a higher proportion of benign neoplastic lesions (73.53% and 71.43% respectively) compared to malignant lesions (26.47% and 28.57% respectively).
Benign neoplastic lesions of sinonasal tract
Maximum benign neoplastic lesions of sinonasal tract in our study were seen in the 31 to 40 years and 61 to 70 years age group. Mane et al9 reported similar findings where benign tumours were reported commonly in fourth decade. Male preponderance was reported in benign neoplastic lesions and this was corroborated by Kulkarni et al,6 Raj et al8 and Mane et al.9
Hemangioma (46.16%) was the commonest benign lesion followed by inverted sinonasal papilloma (38.46%), angiofibroma (7.69%) and trichoepithelioma (7.69%). Kulkarni et al6 observed that the most common benign neoplastic lesion of sinonasal tract was hemangioma (38.46%) followed by angiofibroma (30.76%). Mane et al9 noted sinonasal papilloma (40%) and Khan et al11 reported angiofibroma (42.85%) as the most common benign neoplastic lesion of sinonasal tract.
Hemangioma
It was noted that hemangioma could occur in any age group but was most commonly noted in the fourth decade. This finding was in accordance with Dasgupta et al12 and Kulkarni et al6 who re ported the same and the mean age of presentation in their studies was 32.4 years. Females were more afflicted than males (1:2). Similar findings were noted by Kulkarni et al6 (1:1.5) but Dasgupta et al12 observed male preponderance (1.95:1). Microscopic fe atures such as lobular arrangement, capillary proliferation and capillary lining by plump endothelial cells were noted. (Figure 4)
Inverted sinonasal papilloma
Mean age of presentation of patients diagnosed with inverted papilloma was 54.6 years which was in concordance with studies by Tondon et al10 and Mane et al.9 Inverted papilloma predominantly affected males in this study (M :F ratio is 4:1). Similar observations were noted by Tondon et al10 and Mane et al9 (M:F ratio 3:1 and 5:1 respectively). Microsc opic examination revealed inverted growth pattern of surface epithelium with intact and distinct basement membrane and loss of submucosal glands. (Figure 5)
Malignant neoplasms of sinonasal tract
Maximum cases of malignant neoplasms of sinonasal tract were observed in the seventh decade of life in the present study. Khan et al11 and Mane et al9 reported maximum malignant neoplasms in sixth and seventh decade. Malignant neoplasms were common in females in the present series (M :F ratio was 1:4.5). Similar fin dings were noted by Raj et al8 (1:1.67) and Mane et al9 (1:2).
The most common malignant neoplastic lesion of sinonasal tract was squamous cell carcinoma (36.37%) followed by malignant melanoma (27.27%), nasopharyngeal carcinoma (18.18%), adenoid cystic carcinoma (9.09%) and T cell lymphoma (9.09%). Studies by Khan et al11 and Raj et al8 also reported squamous cell carcinoma as the most common malignant lesion but Mane et al9 reported sinonasal undifferentiated carcinoma as the most common malignant sinonasal tract lesion. Other malignant neoplastic lesions diagnosed in this study showed varying frequencies or were not noted at all.
Squamous cell carcinoma
The age range of patients with squamous cell carcinoma observed was 18 to 65 years and the mean age of presentation calculated was 39.5 years. Dasgupta et al12 noted the mean age of presentation as 52.3 years for patients suffering from sinonasal squamous cell carcinoma whereas Khan et al11 reported peak incidence of squamous cell carcinoma in the sixth and seventh decade of life. We found that only females were affected by squamous cell carcinoma. However, Dasgupta et al12 and Khan et al11 noted a male predominance (2:1). This variation can be attributed to the small sample size (4 cases) in our study. On microscopy, infiltrating nests of squamous epithelial cells were noted. The epithelial cells were highly pleomorphic with hyperchromatic nuclei, nuclear atypia and abnormal mitotic figures. Keratin pearls were observed.
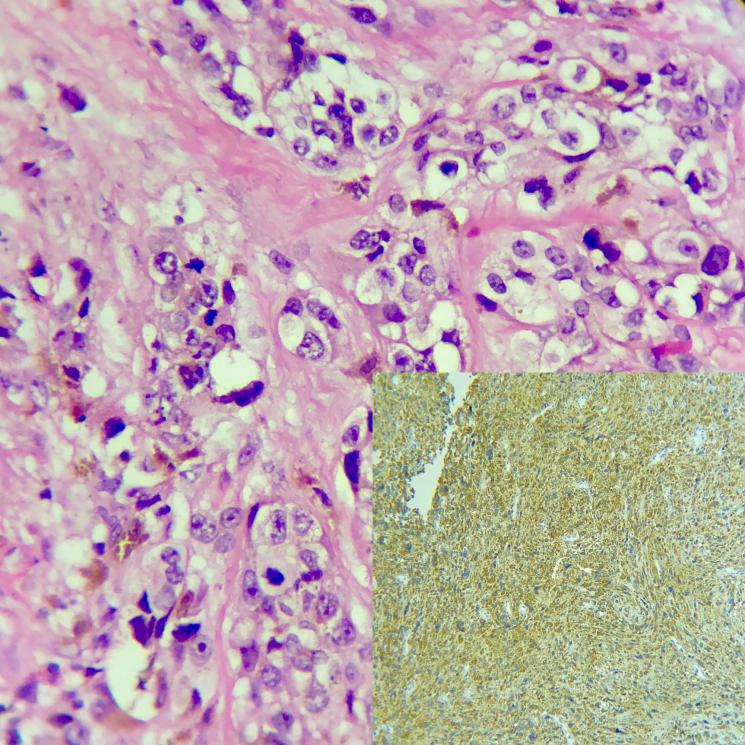
Malignant melanoma
Peak incidence of malignant melanoma was in the seventh decade. Khan et al11 noted maximum cases in the fourth decade. In the current series, all malignant melanoma cases were females. Khan et al11 noted equal sex distribution. Microscopic examination revealed atypia of melanocytes with prominent nucleoli and mitotic activity. On immunohistochemistry, neoplastic cells showed reactivity for HMB-45 and S-100. (Figure 6)
Conclusion
To conclude, various types of lesions affect the sinonasal tract. These lesions can affect any age group. Irrespective of their etiology, whether non-neoplastic or neoplastic, the lesions can present with similar clinical features. Radiological studies and other investigations can help provide a differential diagnosis, but the final diagnosis can only be given on histopathological examination. Definite diagnosis is essential for further management and to determine the prognosis of the patient. Therefore histopathology plays an intergral role and remains the gold standard for establishing the diagnosis of sinonasal tract lesions.