Introduction
Papulosquamous lesions are a heterogenous group of dermatological conditions characterized by formation of papules which coalesce to form plaques.1 The lesions are generally erythematous and they tend to for m scales. Even though they are morphologically similar, the underlying etiology remains varied. Thus, clinical examination and diagnosis of the cases is often confusing. The underlying causes are varied including genetic disorders, inflammatory, infectious, and neoplastic disorders. These diseases are also important because of their greater frequency of occurrence.
The confirmation of the diagnosis by histopathological examination remains the gold standard.2 Specific histomorphological findings in correlation with the clinical features gives a conclusive diagnosis. This is very much necessary as the treatment and prognosis of different conditions is varied.
The papulosquamous disorders include relatively common conditions like psoriasis, lichen planus, pityriasis rosea, parapsoriasis, pityriasis rubra pilaris, lichen nitidus, lichen striatus, prurigo nodularis, mycosis fungoides and infections like tinea corporis.
The aim of this study is to have a view of the spectrum of lesions that we come across the umbrella of papulosquamous lesions, their sex and gender prevalence, and to have a deep insight into the histopathological features of the various pap ulosquamous conditions.
Materials and Methods
The present study is a prospective study comprising of 70 cases of non infectious papulosquamous skin diseases who consulted Department of Dermatology at Mediciti institute of medical sciences during a period of one year from June 2017 to July 2018. Patients history and relevant clinical details were provided by the dermatologist. Wedge biopsy was taken under local anaesthesia.
The tissue was immediately fixed in 10% formalin, processed and embedded in paraffin blocks after which sections were cut and subsequently stained with Hematoxylin and Eosin.
The stained sections were systematically evaluated in weekly clinicopathological conference held in department of pathology in collaboration with dermatology department.
Results
The present study comprised of 70 cases of skin diseases presenting as papulosquamous lesions. Majority of cases were in the age group of 31 to 40 years (16 cases, 22.8%) followed by 11 to 20 years (15 cases, 21.4%). Females were more commonly affected with 37 cases(52.8%) compared to males with 33cases (47.1%) and female to male ratio of 1:0.89.
Table 1
| Age group(years) | Number | Percentage |
| <10 | 1 | 2% |
| 11-20 | 15 | 21% |
| 21-30 | 9 | 13% |
| 31-40 | 16 | 23% |
| 41-50 | 14 | 20% |
| 51-60 | 10 | 14% |
| >60 | 5 | 7% |
Age distribution in papulosquamous lesions
In the present study, out of 70 cases, 34 cases (48.5%) were diagnosed as psoriasis, Lichen planus- 15 cases(21.4%), Chronic Dermatitis- 4 cases (5.71%), Lichen striatus- 3 cases (4.28%), Pityriasis Lichenoides- 2 cases (2.85%), Pityriasis Rosea- 2 cases(2.85%), Prurigo Simplex- 2 cases (2.8%), Prurigo Nodularis and Lichen Nitidus 1 case each, Normal skin 3 cases, 1 case each of atopic eczema, contact dermatitis and chronic actinic dermatitis.
Table 2
Correlation of histopathological diagnosis with clinical diagnosis
Discussion
In the present study majority of cases were in the age group of 31-40 years.2 Females were more commonly affected.3
Psoriasis was most common disease accounting for 48.5%(34 cases) which was most commonly seen in the age group of 41-50 years. This was in accordance with Griffith et al study and Bell et al study. But most studies like Karumbaiah et al and Parvathi et al quote that the age of incidence 20-40 years. Worldwide statistics show that psoriasis is more common in male. But our study had female preponderance with 20 cases occurring in females in contrast to 14 cases in males.3
Psoriasis vulgaris presented as erythematous, well defined plaques with scales.
Histopathological findings showed hyperkeratosis in 7 cases (20.6%), parakeratosis in 20 cases (68.8%), acanthosis in 26 cases(73.6%) with fusion of rete pegs, suprapapillary thinning in 13 cases(38.2%). Hypogranulosis in 4 cases(11.7%), munro microabscess in 5 cases(14.7%), spongiotic pustule of Kogoj in 1 case (3.3%). Derma l changes showed papillary oedema in 2 cases(6.8%), perivascular lymphocytic infiltrate in 17 cases(60%) and dermal infiltrate of lymphocytes in 6 cases (17.6%).
These findings were in correlation with Karumbaiah et al which also showed Acanthosis as the predominant finding in histopathology of psoriasis accounting to its presence in 86.36% and Chavhan et al which also showed acanthosis as the predominanat finding accounting to its presence in 90% of cases. Presence of Munro microabscess and spongiform pustule of Kogoj was less in the present study accounting for around 3% which was in accordance with other studies like Balaji et al and Karumbaiah et al.1
Table 3
Histopathological features of psoriasis
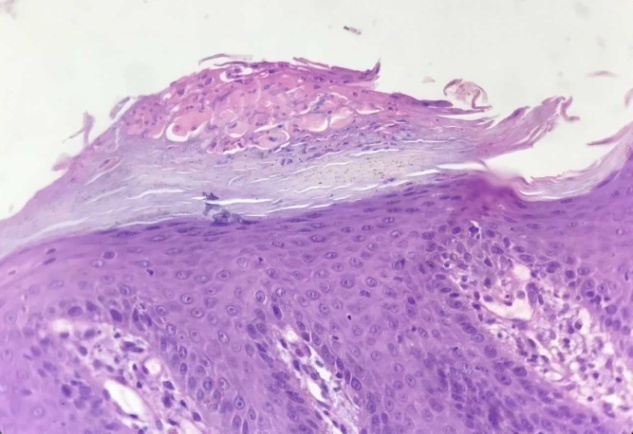
Figure 2
Histopathology of psoriasisFigure 2 H & E section(10x) shows a) Focal parakeratosis b) Focal hypogranulosis c) Irregular acanthosis with suprapaillary thinning d)Regular elongation of rete ridges e) Dilated and tortuous blood vessels in papillary dermis.

Figure 3
Histology of munro microabscessFigure 3 H&E, 40X section shows accumulation of polymorphonuclear cells in stratum corneum- Munro’s Microabscess.
In the present study, 4 cases of clinically diagnosed psoriasis showed different pictures on histopathology. The histopathological diagnosis for these four cases were - 2 cases of atopic dermatitis, 1 case of contact dermatitis and 1 case of palmoplantar keratoderma. Reasons for non correlation being considerable overlap in clinical presentation, partially treated or recurrent lesions were presenting with overlapping clinical features. Due to Kobners phenomenon psoriasis can develop within areas of contact dermatitis.
In the present study, Lichen planus is the second most common lesion accounting for 15 cases (21.4%) Lichen planus cases occurred in 9 females and 6 males with female preponderance. This was in accordance with Balaji et al. The predominant age of presentation is in the 3rd decade with a wide age of presentation 20-50 years. This was in accordance with Karambaiah et al and Balaji et al.4
Lichen planus presents as flat topped, violaceous to erythematous lesions. Histopathology findings show hyperkeratosis in 4 cases(40%), hypergranulosis in 2 cases (20%), irregular acanthosis with saw toothed rete pegs in 6 cases (60%), vacuolar degeneration of basal layer in 8 cases(80%), civatte bodies in 2 cases (20%), band like infiltrate in papillary dermis in 10 cases(100%) and pigment incontinence in 3 cases(30%). This was is in accordance with Karambaiah et al.1
Table 4
Histopathological findings in lichen planus
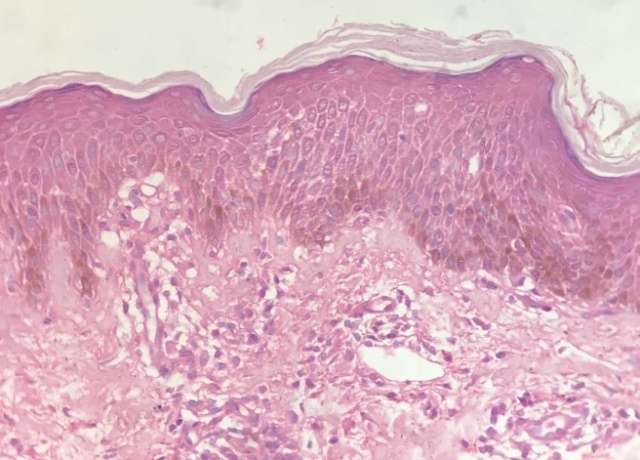
Figure 4
Histopathology of lichen planusFigure 4 H& E, 10X Section shows a) Irregular acanthosis b)Basal Cell degeneration c) Saw tooth rete ridges d)Dense band like mononuclear cell infiltrate in upper dermis e)Pigment incontinence.

Of the 15 cases of lichen planus 10 cases were classical lichen planus, 2 cases were hypertrophic lichen planus and 1 case of lichen planus pigmentosus. Only 2 cases did not correlate with the histopathological diagnosis. These 2 cases were diagnosed as post inflammatory hyperpigmentation on histopathology as they were showing melanophages in superficial dermis, with lymphocytic infiltrate in the surrounding dermis. The non correlation was due to clinical overlap of presentation.
3 cases of Lichen striatus were seen to be confirmed on histopathology. The cases labeled as lichen striatus showed lichenoid reaction confirmed only to few papillae with focal dyskeratosis. These three cases were mostly seen in males in the adolescent age. But 1 case was seen in a 33year old patient. This was in concordance with studies done Mittal R et al.5
1 case of lichen nitidus was seen which was confirmed on histopathology. The histopathology showed classical delling of the epidermis with claw shaped elongation of rete ridges encircling an infiltrate. This single case occurred in a male patient. The age of presentation is 11 years for this patient. This is a rare condition occurring in young children.
There were 2 cases of Pityriasis lichenoides chronia. Only one case was correlated clinically but the other turned out to be lichen planus on histopathology. Out of the two cases 1 case was seen in male patient and other in a female patient. The age of presentation in the female patient was 22 years which correlated with the histopathological findings. The histopathological findings in pityriasis lichenoides were basal cell vacuolations, mild spongiosis and exocytosis of mononuclear cells with perivascular dermal infiltrates.6
There were 2 cases of pityriasis rosea which were confirmed on histopathology. These cases occurred in female patients in their third decade. There was spongiosis with parakeratosis on histopathology.7
Figure 6
Histopathology of pityriasis roseaFigure 6 H&E, 40X, Section shows a) Decrease in the granular cell layer b) Spongiosis c) Mild acanthosis
There were 2 cases of prurigo simplex. Both were confirmed with histopathology. The 2 cases occurred in male patients of 33 years and 71 years of age. The histological findings were parakeratosis, mild acanthosis, pongiosis mostly around the hair follicle.
There was 1 case of prurigo nodularis which was seen in a female patient of 18 years. It was confirmed on histopathology which showed irregular acanthosis and dermal infiltrate of lymphocytes and eosinophils
There is 1 case of atopic dermatitis, chronic actinic dermatitis and contact dermatitis.
Atopic dermatitis case correlated histopathologically showing more of acanthosis, dilated papillary dermal blood vessels and presence of eosinophils in the dermis. This case occurred in a female patient of age 17 years.8
Chronic actinic dermatitis case also correlated well with the histopathology which occurred in a 60 year male patient. The histopathology shows acanthosis, mild spongiosis and lymphocytic exocytosis.
Contact irritant dermatitis also correlated well with the histopathological findings showing spongiotic vesicle formation with disintegrated keratinocytes and neutrophils within it. This case occurred in a female patient of age 65years.
However 3 cases were inconclusive as we could see only normal appearing epidermis and dermis. Reasons can be due to wrong biopsy site or biopsy from already treated case.
Table 5
Non correlated cases of the papulosquamous lesions in the present study
Thus most of the cases had a good clinicopathological correlation. The main causes for non correlation were partly treated cases, considerable overlap with clinical diagnosis, and improper history of the patient. But with good clinical data the difficulty can be evoked to some extent in coming to a proper final diagnosis.
Conclusion
Papulosquamous lesions are the most common and distinct varity of skin lesions. These generally affect the adult females. Psoriasis and Lichen planus constitute the bulk of the papulosquamous lesions. Specific histological features for the diseases help us to come to conclusive diagnosis. However few cases pose diagnostic problems even after histopathology which can be solved with a good clinicopathological correlation.


