Introduction
HIV (Human immunodeficiency virus) infection and its resultant AIDS (acquired immune deficiency syndrome) have become a global pandemic.1 In 1981, AIDS was first recognized in United States. In 1983, HIV was isolated from lymphadenopathy patient, and demonstrated to be the causative agent of AIDS in 1984.2 HIV disease can be classified as per immunodeficiency into an early stage [cluster of differentiation (CD)4 > 500/ μL], an intermediate stage (CD4 = 200-500/ μL), and an advanced stage (CD4 < 200/ μL).4, 3
The major anatomic site for establishing and propagation of HIV infection are lymph nodes, which form the bulk of lymphoid tissue. Lymphadenopathy may also be a manifestation of opportunistic infections, lymphoid malignancy developing in an immunodeficient individual but it is one of the initial manifestations of HIV.6, 5 The most useful diagnostic procedures for HIV patients with lymphadenopathy are lymph node biopsy (Gold standard), but the method has several disadvantages.7
FNAC can serve as conveniently substitute method practiced for the diagnosis of opportunistic infection in HIV/AIDS, for example Toxoplasmosis, Histoplasmosis, Tuberculosis and malignant condition like Kaposi’s sarcoma and lymphoma.8 In the assessment of lymphadenopathy particularly in HIV-positive patients, FNAC method has become the primary investigative procedure. This process is fast and easy to accomplish and sometimes can be avoided excision while monitoring the following therapy.9 The use of a simple investigative tool to rapidly identify the cytomorphological patterns in lymphadenopathy of seropositive cases, and in turn initiate therapy directed specifically towards the disease can help reduce the already excessive burden on HIV patients.
Hence, current investigation was carried out to assess the role of FNAC as a cytological diagnostic measure for the judgment of numerous lesions in HIV lymphadenopathy and correlate its findings with serum CD4 counts.
Materials and Methods
After obtaining Institutional Ethical Committee approval and written informed consent from the patients, the hospital based cross sectional study was carried out over a period of one and half year in Pathology department of Tertiary Health Care Centre. A total 75 cases of all genders and age, already diagnosed as seropositive by ELISA and presented with lymphadenopathy of ≥ 1 cm were involved in the study. Patients who are not agreeable to contribute in the study were excepted from the study.
A detailed clinical history of patient was recorded in a set proforma including the demographic data, history of acquiring and first diagnosis of HIV/AIDS. A detailed and thorough clinical examination including the general examination and specific examination of palpable lymph nodes was done. Sites for lymph node aspiration were Cervical, Axillary, Inguinal and any other.
All HIV positive patients having lymphadenopathy were subjected to FNAC in pathology department of cytology OPD. The inflammation was localized by cautious palpation and position was cleaned with spirit and fixed in a favorable site with one hand. A 23 or 24 gauge needle was attached to a 20cc syringe fitted with comeco syringe pistol. The needle was inserted through the skin with quick motion and advanced into the swelling. By noting the resistance encountered on puncture, it was ensured the needle was in lymph node. After puncturing swelling negative pressure was produced by withdrawing the nozzle of pistol. The needle was moved to and fro within node maintaining negative pressure. Once aspirate was observed at the junction of needle and hub, aspiration was stopped by releasing vacuum in syringe. The needle was withdrawn from the lymph node, content of needle carefully expressed on to the glass slide. Smears were prepared with use of flat surface of another slide by applying pressure. Smears were instantaneously fixed in 95% ethanol for PAP staining. 10 Air dried smears were reserved for MGG.10 and AFB.10 The serum CD4 count of the patient was assessed by BD FACS Count System (immunocytometry system).11
Data analysis
Data collected was entered simultaneously into “Statistical Package for Social Scientists” (SPSS) software version 17.0 and coded appropriately. Results are presented in the form of tables, pie chart and bar diagrams. Findings were compared against findings from similar studies and discussed.
Observations and Results
Total 75 HIV positive patients were involved in the study, amongst them 43 (57.3%) were male and 32 (42.7%) were female suggesting a male prevalence. The ratio of male:female comes out to be 1.3: 1. Most of the male patients were between 31-40 years age group (17.3 3%) and females were in between 21-30 years age group (20%), (Table 1).
Table 1
Distribution of cases as per age and sex
Most of the cases had involvement of cervical lymph nodes i.e. 60 (80%) followed by axillary 6 (8%) and others [(12%) (Supraclavicular 4%, Sub mandibular 2.7%, Inguinal 1.3%, Post auricular 1.3%, Pre auricular 1.3%, Submental 1.3%)].
Commonest cytological diagnosis was chronic granulomatous lymphadenitis seen in 30 cases (40%), subsequently tuberculous lymphadenitis 36% (27). The reactive lymphadenitis is reaction to any foreign antigen while non-specific lymphadenitis is a type of reactive which may be long standing. In current study reactive lymphadenitis was seen in 14 cases (18.6%). 2.7% each accounted for acute suppurative lymphadenitis and non-specific lymphadenitis (Figure 2). The most common cytomorphological pattern identified amongst tubercular lymphadenitis was smears viewing caseous necrosis with epithelioid cells with total 15 (55.5%) out of 27 cases. 3 cases (11.1%) were found with Suppurative features. Only seven cases (26%) had smears showing caseous necrosis while 2 (7.4%) had epithelioid cells.
In all the patients serum CD4 cell count was carried out and compared with the cytological pattern as shown in table 2. In 8% (6) cases of reactive lymphadenitis was observed serum CD4 count of > 500 cells/ μL and 2.6% (2) cases of chronic granulomatous lymphadenitis. In 13.3% (10) cases with tubercular infection had serum CD4 count of 200 – 499 cells/ μL and 22.6% (17) cases had serum CD4 count of <200 cells/ μL. Twenty cases of chronic granulomatous lymphadenitis was found 200 – 499 cells/ μL of serum CD4 count and 8 cases had < 200 cells/ μL serum CD4 count
Table 2
Comparison of CD4 count with several cytological diagnoses
Figure 4
Photomicrograph viewing group of a): epitheloid cells (LP, H&E) and b): epithelioid cells (HP)
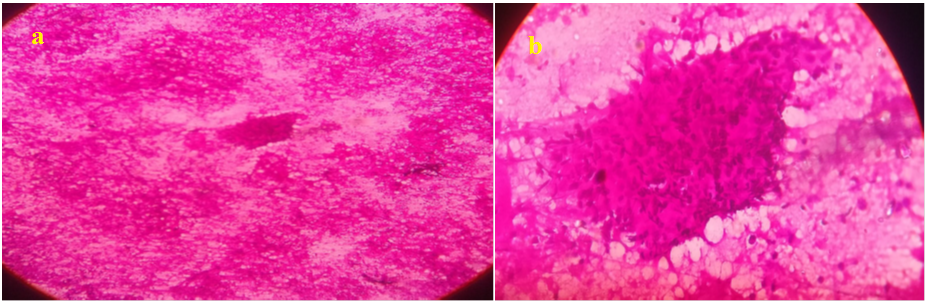
Figure 5
Photomicrograph viewing mixed population of lymphoid cells, centroblasts, and centrocytes, large and small lymphocytes a): (LP, MGG) and b): (HP, MGG) (Reactive lymphadenitis)
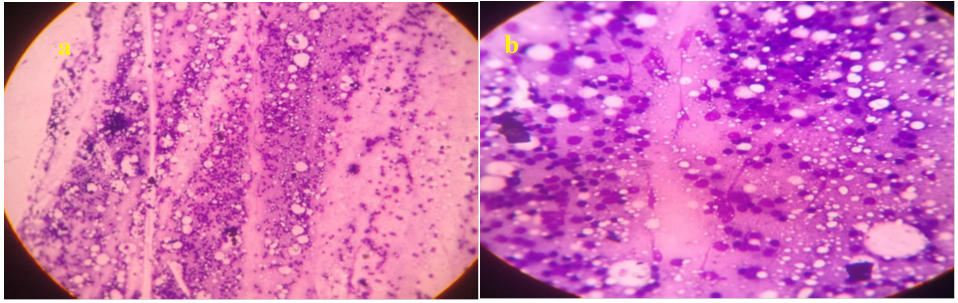
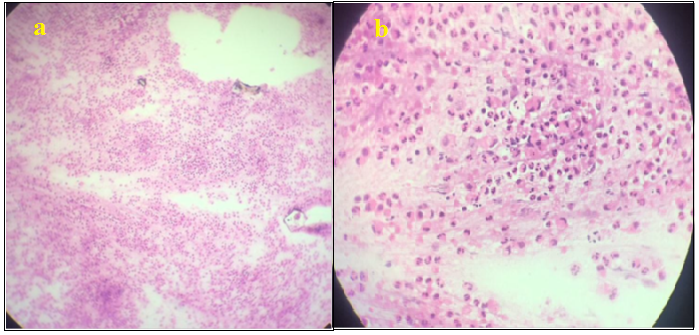
Figure 6
Photomicrograph viewing dense infiltration of neutrophils a): (LP, H&E) and b): (HP, H&E) (Acute suppurative lymphadenitis)
Discussion
In present investigation, the prevalence of HIV lymphadenopathy was more observed in males particularly in 4th decade of life and majority of females of 21-30 years age group. Many HIV patients had involvement of cervical lymphadenopathy followed by axillary. Our study correlated well with the previous studies.13, 12, 7, 6, 5 Chronic granulomatous lymphadenitis is the most common cytological diagnosis which is quite in contrast to other studies conducted in the Indian subcontinent,17, 16, 15, 14 where the main contributor was mycobacterial infection. This could suggest an increased incidence of HIV positive patients already on HAART and Anti Tubercular drugs before presenting with lymphadenopathy in cytology OPD, therefore showing paucity of AFB on smears. However, Reid et al18 also had a lesser incidence of mycobacterial cases which may be due to less overall incidence of tuberculosis as an opportune pathogen. This study had reactive lymphadenitis as the most common diagnosis (51%), whereas the present study had only 18.6% cases with reactive findings. No cases of lymphoma were found in the current study.
In tuberculous lymphadenitis cases, the most common cytomorphological pattern was caseous necrosis with epithelioid cells and another common pattern was caseous necrosis in contrast to Surase et al16 where the second most common was epithelioid cells only. 3 of the total 27 tuberculous lymphadenitis cases showed features of acute suppuration with positive Ziehl Neelson staining. Simil ar findings were seen in study done by Kumarguru et al5 and Gorva et al.13
Serum CD4 cell count was available for all the participating patients on whom FNAC was performed. Most of the cases of chronic granulomatous had 200-499 cells/ μL serum CD4 count with a mean of 330.2, t his finding was quite similar to that of Agravat et al;14 while 8 cases had <200 cells/ μL serum CD4 count. Tubercular lymphadenitis cases did not observed above 500 cells/ μL serum CD4 count, which may suggest a depression in the immune system and the presence of an opportune infection, this is correlated well with finding of Deshmukh et al.17 The least mean value of serum CD4 count was seen in this particular category was 118.29 cells/ μL, which was close to a study by Kumar et al19 where necrotizing suppurative lymphadenitis accounted for the most common cytomorphological finding amongst the tubercular group with a mean serum CD4 count of only 92cells/ μL. Those patients with a reactive lymphadenitis did not show less than 200 serum CD4 value. Among 14 cases, 6 (42.8%) had a serum CD4 count of >500 cells/ μL (mean = 633 cells/ μL) and 8 (57.14%) had a value between 200–499 with a mean of 323.3 cells/ μL. Reactive lymphadenitis was the only cytological diagnosis which showed such a high mean value of serum CD4 count. These results are comparable with the study done by Deshmukh et al17 and Pista et al.20
Only two cases of acute suppurative lymphadenitis were identified, both having a serum CD4 cell count between 200 – 499 cells/ μL (mean = 220.5). Similarly, only two cases of non – specific lymphadenitis were diagnosed with extremes of serum CD4 value. One had a value of 52 cells/ μL and the other with a value of 551 cells/ μL. Hence, no definitive interpretation of this finding could be established.
Conclusion
FNAC of lymph node is very helpful in segregating cases that need further assessment. One of the major opportunistic infections detected in both symptomatic as well as asymptomatic patients was Tuberculosis. Therefore, ZN staining should always be done for detection of AFB in spite of the cytological picture not suggesting it. Correlation of cytological diagnosis with serum CD4 T lymphocyte count gives invaluable information regarding stage of the disease and immune status.
Hence, FNAC is the easy and very effective diagnostic modality for HIV lymphadenopathy patients. It helps in the identification of majority of the granulomatous, reactive, and opportunistic infections. It therefore, helps in guiding subsequent management of these patients.



